Alzheimer’s disease is deeply intertwined with gender inequalities. Women make up the majority of those who develop the disease, and at the same time, they are most of the caregivers for these individuals. Since age is the main risk factor, one might think that women’s longer life expectancy could explain the higher number of cases. However, the reality is much more complex: men and women face different exposures to risks, brain pathologies, and levels of resilience to Alzheimer’s.
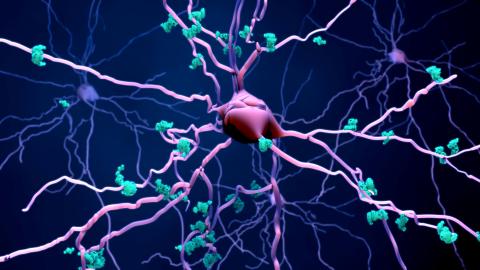
This neurodegenerative disease is, in most cases, a condition caused by a combination of genetic and environmental factors. This means there is no single determining factor that explains the development of the disease. Biologically, it is characterized by the deposition of amyloid and tau proteins inside and outside neurons, respectively. Neurons are the brain cells that act as "messengers," receiving, processing, and transmitting information to other neurons. This way, they form a network that supports mental abilities such as memory. Amyloid and tau pathologies disrupt the functioning of these networks, leading to the disease’s symptoms: a progressive decline in mental abilities, and ultimately, dementia.
Alzheimer’s disease is deeply intertwined with gender inequalities. Women make up the majority of those who develop the disease, and at the same time, they are most of the caregivers for these individuals
Currently, we understand that up to two decades may pass from the onset of biological changes in the brain to the manifestation of mental ability problems, known as symptoms. During this long period, there are opportunities to influence the disease’s progression. Previous studies have investigated how to slow the accumulation of amyloid and tau proteins to increase resistance to the pathology. Alternatively, other studies have focused on understanding how to strengthen neurons’ ability to adapt to the accumulation of pathological proteins and maintain their function, which is known as resilience to the disease.
Resilience against the development of dementia
What can help increase resistance and resilience against the development of diseases like dementia? There are 12 recognized risk factors that increase the likelihood of developing dementia and could account for up to 40% of cases. These factors include education level, physical activity, and depression, among others. Improving these aspects can significantly influence the development of the disease, offering greater protection and adaptability of the brain. But what is the role of sex and gender in disease resilience? The prevalence of protective and risk factors –the burden of Alzheimer’s pathologies—, differs according to sex and gender, as in biological factors versus socially constructed ones.
Sex refers to the sex-chromosome pairing of a person (XX vs. XY, female vs. male sex), which is reflected in reproductive organs. In contrast, gender is a social construct that refers to socially constructed roles, identities, and behaviors. Gender is complex and changing, as it is influenced both by social and cultural contexts of the past and by current ones. This binary approach (female/male, woman/man) has limitations, but it is the approach predominantly used in research to date.
What do studies show about the role of sex and gender in resilience? A sex and gender perspective in Alzheimer’s disease implies understanding that the female sex may be associated with greater protein accumulation, while historical patterns of gender inequality may also be contributing to the higher risk of Alzheimer’s in women.
A sex and gender perspective in Alzheimer’s disease implies understanding that the female sex may be associated with greater protein accumulation, while historical patterns of gender inequality may also be contributing to the higher risk of Alzheimer’s in women
Women initially cope better with pathology and the loss of neurons or neural connections, maintaining their mental abilities. Thus, women show greater resilience to the early changes of the disease. For example, this greater initial resilience in women could be partially explained by the female sex, as research with animals (in which sex chromosomes can be manipulated in the laboratory) shows a protective role of the X chromosome in Alzheimer’s disease. However, women’s mental abilities decline faster than men’s as the disease progresses.
Thus, initial resilience in women tends to fade as their mental abilities begin to deteriorate, which progressively leads to an Alzheimer’s disease diagnosis. Here, biological sex also seems to play an important role, as in menopause (associated with the female sex) there is greater accumulation of tau protein in the brain and there is a greater presence of other brain pathologies (like vascular ones), all of which contributes to a greater neuronal damage.
Evaluating how sex and gender interact is crucial
It is important not to overlook how gender roles can influence the risk of a disease. Some conditions that increase risk are more common in women, including low levels of education, physical inactivity, and affective disorders (inevitably linked to caregiving).
In fact, different research indicates that, in countries with less gender inequalities, the differences in mental abilities are decreasing between women and men. Women have been less encouraged to exercise and study, leading to a higher prevalence of physical inactivity among them and a lower education level compared to men. Previous studies have shown that physical activity is related to lower amyloid protein accumulation in the brain. Additionally, people with higher educational levels, as well as those who engage in mental activities, tend to have a greater volume of neurons in old age. On the other hand, depression and stress could have a negative effect, potentially reducing the number of neurons and accelerating the accumulation of harmful proteins.
Evaluating how sex and gender interact is crucial to understand the mechanisms that preserve mental abilities and reduce the accumulation of pathologies during aging, thereby preventing Alzheimer’s disease. Sex and gender intersect with other socially constructed concepts, such as "race" and ethnicity, which are essential for understanding and addressing inequalities in disease development.
In the article published in Alzheimer’s and Dementia: The Journal of the Alzheimer’s Association, a group of international expert researchers, including myself, have emphasized the urgency of incorporating a sex and gender approach in studies on Alzheimer’s disease. If men and women develop Alzheimer’s disease through different mechanisms, understanding these mechanisms is essential for designing specific interventions and effectively treating the disease.