What happened?
A publication in Science has uncovered a possible case of fraud in a major line of Alzheimer's research. The alarm was raised by Matthew Schrag, a neuroscientist and neuroscientist at Vanderbilt University, and the journal itself continued the analysis. Specifically, they identified that there were all sorts of image manipulations in at least ten articles on the so-called Aβ*56 peptide. All of them included the byline of neuroscientist Sylvain Lesné.
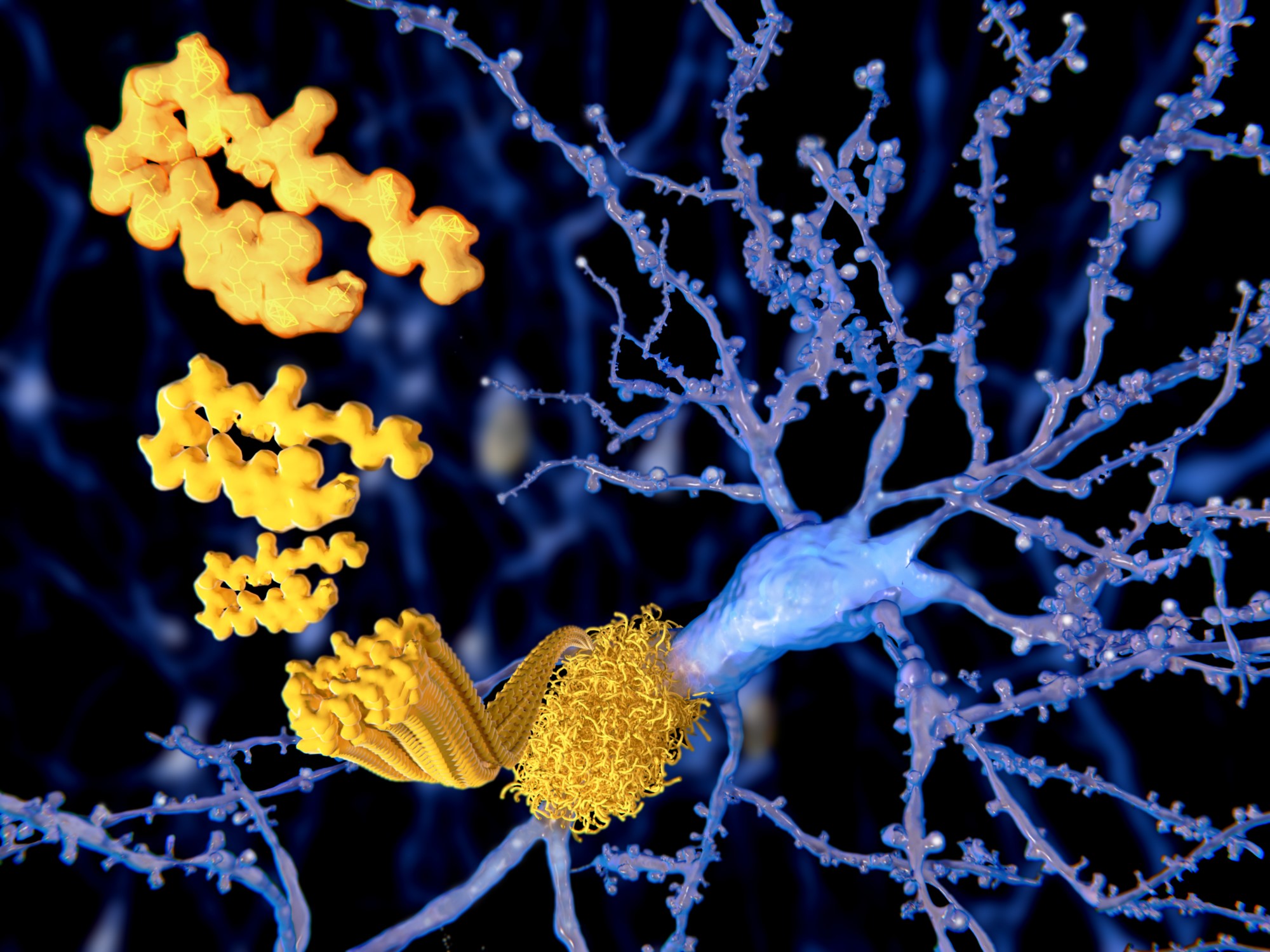
Aβ*56 is a form in which the beta-amyloid protein, the substance that is found forming plaques in the brains of Alzheimer's patients and which, according to the dominant theory of the last decades, is responsible for initiating the disease, can occur.
One of these ten papers is one of the most cited in the history of Alzheimer's research. Published in Nature in 2006, it claimed that injecting the Aβ*56 form into healthy rats caused them to develop memory loss. It was the first time that a substance, theoretically present in the brains of people with Alzheimer's disease, had been shown to directly cause these symptoms. It was an endorsement of the amyloid hypothesis.
Schrag avoids the term "fraud" in his criticism and describes his findings as a "wake-up call". Other experts consulted by Science magazine call them "striking examples of image manipulation". Many other groups are also said to have tried unsuccessfully to reproduce the results, but very few reported them. Although an irreproducible result does not necessarily imply fraud, the article acknowledges that there is little interest in negative results and it is difficult to contradict authoritative researchers.
Juan Fortea, neurologist at the Memory Unit of the Neurology Service of the Hospital de la Santa Creu i Sant Pau in Barcelona and coordinator of the Study Group of Behavioural Neurology and Dementias of the Spanish Society of Neurology (SEN), tells SMC Spain that there may have been malpractice. "It seems that we are indeed facing a case of fraud or scientific malpractice because of what has been published, although we must be cautious until the investigations underway by the university with which the principal investigator of the research is affiliated are concluded".
Following the publication, some articles and multiple comments on social media claimed that all Alzheimer's research was based on fraud and that hundreds of millions of euros and decades of effort had been wasted. However, many experts have tried to disprove these findings and put their impact in context. It is all about the beta-amyloid protein.
What is β-amyloid
These are small fragments that come from the so-called amyloid precursor protein. There are many different forms that tend to aggregate and end up forming the plaques characteristic of Alzheimer's disease. In the case of Aβ*56, it would be what is called a soluble oligomer, a form that is presumably toxic but is not found forming part of the plaques.
This is a simple chronology of some important findings:
- Between 1906 and 1911, Alois Alzheimer (and Oskar Fischer) begin to describe the characteristic plaques of sufferers.
- In 1984 it is established that the β-amyloid protein is the main component of plaques.
- In 1991, it began to be published that several mutations that increase the amount of amyloid precursor protein inevitably cause the disease in those who carry them. It is assumed to be the cause of Alzheimer's and the theory becomes dominant.
Does the possible fraud disprove the amyloid and Alzheimer's theory?
No. In the words of Alzheimer's researcher Karl Herrup on Twitter, "the scale of the fraud is shocking, but the importance to the Alzheimer's field has been grossly exaggerated". According to chemist Derek Lowe, a former Alzheimer's researcher who runs a blog in the journal Science, "it certainly increased enthusiasm and funding levels in the area and gave people more reason to believe". However, the Aβ*56 work now in question "did not lead directly to any clinical trials in that particular form". Too many eggs were probably put in the same amyloid basket, but it was not triggered by these papers.
These papers were a boost, but they are just one branch on the whole theory tree. Also on Twitter, researcher Samuel Marsh explained that "the main paper in question did not establish the amyloid plaque model. It talked about a specific oligomer called AB*56. There are many other papers in the field that show the importance and effects of oligomers and plaques". He continued: "I sincerely doubt that the absence of this particular paper and AB*56 from the historical scientific record would have significantly changed the last 20 years of drug development for Alzheimer's disease. That's because there is strong genetic and other evidence for the role of amyloid in the disease.
For John Hardy, discoverer of one of the mutations that inevitably leads to the disease, "it is a disgrace that these papers involve deception, and journals and institutions should take action against fraud when it is discovered". However, "I have never thought this article was important, and I don't think I have ever referred to it in my own work".
Juan Fortea's opinion is along the same lines. For the neurologist, "this work is not a pillar of the amyloid cascade hypothesis, which was formulated years before the appearance of these publications by this author. The hypothesis is based primarily on genetic evidence linking amyloid processing to Alzheimer's type dementia". "That is why I believe that the anti-amyloid trials would have been carried out anyway, even without these publications being challenged," he adds.
The amyloid theory was already controversial before this case. Why?
In recent years there has been intense debate about the relevance of amyloid in Alzheimer's disease. One reason is that quite a few elderly people have amyloid plaques, but no symptoms, so amyloid may not be enough to develop the disease. On the other hand, and this is the main reason, although clinical trials designed to reduce plaques have repeatedly succeeded in reducing them, they have invariably failed to improve symptoms. Even those trials conducted early and in people carrying mutations that cause them to develop the disease in the future have failed to show any improvement.
There is currently only one anti-amyloid drug approved for Alzheimer's, aducanumab. It was given the green light in the US amid huge controversy, both over the bizarre conduct of the clinical trials and the final decision. In Europe, the European Medicines Agency refused to approve it on the grounds that it had not demonstrated clinical benefit and was not sufficiently safe.
Fortea acknowledges that "the amyloid hypothesis has concentrated a good part of the resources allocated to clinical trials, and some/many researchers find it excessive. Beyond the controversy raised by the approval of aducanumab by the US FDA, in the next six months several clinical trials with various anti-amyloid antibodies will be completed which, if they are concordant in one way or another, may dispel the doubts about this therapeutic approach". In any case, for Fortea, "it cannot be said that the trials with anti-amyloid antibodies have shown that they do not work (at least not until these trials are completed). And he adds: "Moreover, even if we were to hypothesise that they were all negative, the incontrovertible genetic evidence [in favour of the hypothesis] would persist. Or to paraphrase Monterroso, the dinosaur will still be there when we wake up. What we do with it in the event that the tests fail is another matter entirely.
What might explain the failure of clinical trials
Some of the explanations that have been put forward are as follows:
- Although logic and genetic studies make it difficult to accept, it cannot be ruled out that amyloid is what is known as an epiphenomenon, something that accompanies the true cause but does not act as such.
- It could be that the treatments included in the trials were not getting there in time. The damage caused by amyloid may be very early, and reducing it once it has triggered the aggression may not be enough. Although some trials have been done in people who are not yet symptomatic, it may still be too late.
- Another option is that the antibodies used to reduce amyloid do not reduce it sufficiently, or that they are acting against certain forms of amyloid that are the really toxic ones. In this case, the total amount would be reduced, but not what is actually causing the damage.
And it is increasingly accepted that Alzheimer's disease is a syndrome, rather than a single disease, and that there are many factors to take into account.
On this particular case, this is how Samuel Marsh ended his explanation: "Ok that’s all for now. Horrible misconduct yes. The reason that AD field has focused on amyloid for past 16 years: absolutely not. This is already a big story but inaccurate hyperbolic reporting makes things worse".
Juan Fortea's conflicts of interest: "I have been a consultant, or have been on advisory boards, for several companies with anti-amyloid antibodies, including Roche, AC Inmune or Novartis and I have given talks for several other companies, including Biogen. However, my main "COI" is scientific, I did my thesis on ADAD (Autosomal Dominant Alzheimer's Disease) and I am the director of an Alzheimer Down unit. These populations are the strongest evidence in favour of the amyloid hypothesis".