Reaction: new technique allows sperm to be selected for sex selection
Researchers in the United States have tested a new technique to select sperm and thereby increase the chances that the embryo will be of either sex. The proven efficacy is around 80 %. Although some countries such as the United States allow this type of procedure, in Spain it is prohibited except in cases of prevention of diseases linked to sex chromosomes. The authors of the article state that sperm selection is more ethically acceptable than embryo selection. The results are published in the journal PLOS ONE.
Rocío Núñez - sexo embriones EN
Rocío Núñez Calonge
Scientific Director of the UR International Group and Coordinator of the Ethics Group of the Spanish Fertility Society
his study on a new sperm sex selection technique is written by one of the leading pioneers in assisted reproduction, Professor Palermo, who is credited with the discovery of ICSI or sperm microinjection. It is a well-designed study, with a high number of cases, of good scientific quality. The journal [in which it appears] does not publish papers that are not of high quality.
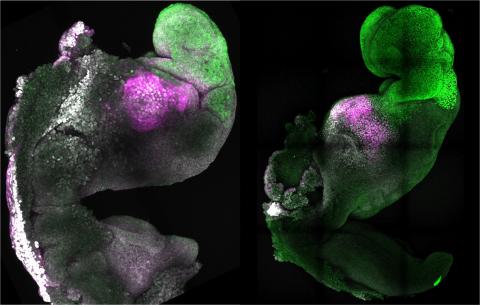
At first, this did not seem to me to be a very novel topic since, as the authors themselves point out, there are many previous studies on the same subject. The novelty lies in [separating] two groups using preimplantation genetic diagnosis (PGT-A) to study chromosomal abnormalities in the resulting embryos, and in one of the two groups using the proposed sperm selection technique. In this way, the researchers compare the two groups to see whether the sex-specific sperm selection technique is useful and safe, and whether further chromosomal abnormalities are found after its use.
The results of the study confirm that it is possible to select a particular sex with a 80% probability, and safely—since the technique, which is very simple, does not affect the genetic load of the embryo.
The authors propose that this technique could be used both for couples who want to select the sex of the baby out of personal desire and for medical reasons—that is, when there is a risk of disease linked to the sex of the baby. They say this would be more ethical than using pre-implantation genetic testing.
From a purely medical point of view, the use of this technique when there is a sex-linked disease (such as haemophilia) would not be appropriate, as an 80% chance leaves the couple with a 20% chance that the baby will not be of the chosen sex, resulting in a person with the disease. However, if the selection is made purely for personal reasons, this margin of error would be acceptable.
In addition, the authors themselves speak of an important limitation, which is that the sex of the embryo chosen for transfer is not known. It may happen that, among several embryos obtained, although most of them are of the desired sex, the wrong one is chosen. From an ethical point of view, what happens to the rest of the embryos that are not chosen? What would be their fate?
Therefore, it does not seem to solve the possible ethical problems that the use of PGT raises.
In Spain, sex selection is not allowed except for medical reasons. When the law was passed in 1988, this issue was raised on the basis of the possible selection that certain groups could make to the detriment of the other sex, which would lead to an imbalance in the population.
At present, such a ban does not make much sense, as sex selection would be performed by a small group of patients for personal reasons, and would not lead to a population imbalance.
The use of the technique proposed by the authors could be very useful in assisted reproduction centres, as it is very simple (almost the same as what is usually done for the preparation of sperm in laboratories), and could help couples who wish to increase the probability of obtaining a child of the desired sex. However, it is only an increase in this probability. [Couples] should be well informed beforehand and not offered any certainties.
Urries - Sexo (EN)
Antonio Urries
Director of the Assisted Reproduction Unit at the Quirónsalud Hospital in Zaragoza and member of the Quirónsalud Scientific Committee
The aim, approach and design of the article is adequate, although its practical usefulness is limited for several reasons. Firstly, its effectiveness is limited (only 80 %) and other procedures with similar effectiveness already exist. On the other hand, it is based on the same principles that have been considered up to now, such as the difference in density between the spermatozoa containing the "X" chromosome and those containing the "Y" chromosome, so it does not provide any differential point in this aspect compared to what already exists. Finally, with regard to the technique used and its reproducibility, it cannot be assessed as it does not indicate the specific technique used. In short, in my opinion, it does not provide added value over and above the social impact that news such as this can have.
I do not agree [as the authors say] that it is more ethically acceptable to make a sex selection through the study of the spermatozoon instead of a diagnosis on the embryo, as I consider that the ethical conditioning factor comes from the concept itself of "à la carte selection", rather than from the technique used. Even from the point of view of its effectiveness, it would currently be more ethical to make the diagnosis on the embryo than on the spermatozoon because of its greater reliability.
We must bear in mind that the Assisted Reproduction Law (Law 14/2006) in Spain considers sex selection without indication as a very serious infraction, with a sanction that can range from 10,001 euros to one million. And it is precisely in this concept of "indication" where the limitation lies. A woman's or couple's wish to have a child of one sex or the other cannot be considered a medical indication. Law 14/2006 on Assisted Reproduction clearly indicated that assisted reproduction should have a clinical indication, and therefore allowed it to be carried out to avoid the transmission of serious hereditary diseases linked to sex, such as haemophilia, muscular dystrophy such as Duchenne or Fragile X syndrome. The rationale was that males had a high probability of manifesting the disease (50%), while females would always be healthy.
It should be noted that at that time we did not know the mutation that caused the disease, so we could not use other more direct procedures, even though we knew that with this sex selection we were also ruling out 50% of males who would have been healthy. This is no longer done in these cases, as we are able to detect the mutation without the need for sex selection. In my opinion, whether or not to allow the application of this type of selection without medical indication should be based on a thorough analysis of the society itself, analysing whether at that moment there could be a population shift towards one or the other sex, as happened in China at the time. An intermediate solution could be to allow the selection of a second child as long as it is of a different sex than the first.
In my opinion, this work does not improve the effectiveness of existing techniques, nor does it provide any novelty in the "basic" procedure, although it cannot be evaluated in detail, since it does not describe the procedure used. We can only highlight the social impact that news such as this can have but which, in Spain, have little chance given the current legislation.
Cheung et al.
- Research article
- Peer reviewed
- Non-randomized
- Clinical trial
- In vitro