Reactions: two studies describe what may be the cells that sustain allergies over time
Two teams of researchers have separately described a population of memory lymphocytes that may be responsible for the persistence of allergies over time. The work has analysed responses to allergens such as those present in peanuts, dust and birch. According to the authors, whose research is published in Science Translational Medicine, these cells could serve as a target for the treatment of various types of allergies.
Dávila - Alergias (EN)
Ignacio Jesús Dávila González
Head of the Allergy Service at the University Hospital of Salamanca, Professor at the Faculty of Medicine of the University of Salamanca and President of the Spanish Society of Allergology and Clinical Immunology
The studies seem to me to be of very good quality, very well thought out and developed.
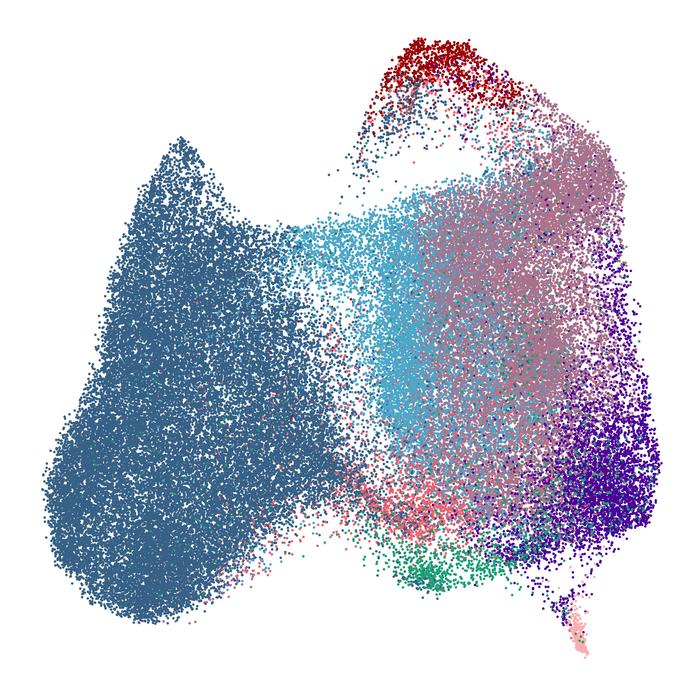
The main issue is that the memory of the immune system for the production of immunoglobulin E (IgE) is not well understood and has focused on plasma cells, many of which are short-lived; however, the production of specific IgE directed against an allergen can be maintained for prolonged periods of time, once sensitisation has occurred. These two studies describe a population of type 2 memory B cells, which express IgG, but also the low-affinity receptor for IgE, FcεRII or CD23, the IL-4 receptor and the IgE heavy chain gene.
Two aspects are important:
- These cells appear to be able to contribute to the production of specific IgE (e.g. against Ara h 2 [the major peanut allergen] in the case of the first study) by differentiating into plasma cells, which could explain the maintenance of very high levels of specific IgE against Ara h 2 in some patients.
- It appears that administration of sublingual immunotherapy may lead to an increase in this cell type as early as one month after treatment, which may also switch to the production of allergen-specific IgG1 or IgG4. The latter is well known to increase with allergen immunotherapy.
Finally, these type 2 memory B cells express the alpha chain of the IL4 receptor and the alpha 1 chain of the IL13 receptor. Blocking these receptors could be an interesting treatment for the induction of tolerance to allergens. Indeed, dupilumab, a monoclonal antibody targeting the IL4 receptor alpha chain and blocking IL4 and IL3 signalling transmission has been shown to reduce total IgE and specific IgE levels and could lead to the development of tolerance.
In terms of limitations, these are initial data that require further confirmation.
He declares that he has no direct conflict of interest with this article, but the following could be indirect: in the last three years, he has received payment for conferences from Allergy Therapeutics, Astra-Zeneca, Chiesi, Diater, GSK, Leti, Novartis, Sanofi; for consultancy, from Allergy Therapeutics, ALK-Abello, Astra-Zeneca, GSK, Merck, MSD, Novartis, Sanofi; and grants in the framework of competitive projects from Thermofisher Diagnostics, ISCIII and Junta de Castilla y León.
África González - alergias EN
África González-Fernández
Professor of Immunology at the University of Vigo, researcher at CINBIO, and member of the RAFG
The study is very complete, of good quality, with a lot of novel experimentation and a lot of bioinformatics. Above all, it is a study carried out on peripheral blood cells in children, with the difficulty that this entails due to the small number of samples that can be obtained from them.
It provides interesting information on the markers and type of IgG+ memory B cells, which would be the cells prior to differentiation into IgE-producing plasma cells highly specific to peanut protein.
The article shows that IgE-producing B cells are not generated directly, but that there has been a class switch from IgM to IgG, prior to becoming IgE+ B cells.
This study confirms in children what had previously been seen in adults, for example in two articles from 2016 and 2020, one with peripheral blood and the other with mucosal cells. It is therefore not entirely novel, but it does confirm what has been observed by other authors.
The only major limitation of the study is that, because they did not have enough sample, they sometimes had to pool cells from several individuals.
Ota et al.
- Research article
- Peer reviewed
- People
Koening et al.
- Research article
- Peer reviewed
- People



