Reactions to trial using CAR-T cells prepared from donors to treat multiple myeloma
Approved therapies to treat various tumours using CAR-T cells are based on the modification of the patient's own lymphocytes in the laboratory, which delays their administration. A phase 1 clinical trial has used ready-made donor cells to treat patients with multiple myeloma. The results are published in the journal Nature Medicine.
Adobe Stock.
José Antonio Pérez - CART mieloma EN
José Antonio Pérez Simón
Head of the Haematology and Haemotherapy Service of the Hospital Virgen del Rocío
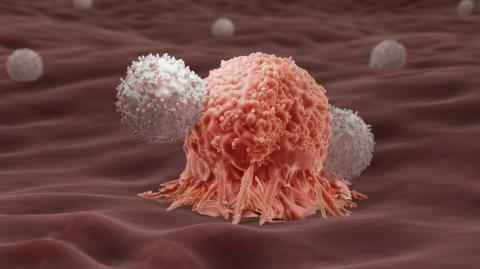
CAR-T lymphocyte therapy is changing the prognosis of patients with various tumours, such as lymphomas or multiple myeloma, when previous lines of treatment have failed. They are manufactured using the patient's own cells which, after manipulation, are able to recognise and selectively destroy tumour cells. Currently, the manufacture of these CAR-T cells is time-consuming and some patients may experience disease progression during this period.
Allogeneic CAR-T cells [from another person] are made from cells harvested from a healthy donor instead of the patient and can be prepared in advance, potentially allowing patients to receive this treatment faster. On the other hand, many patients' immune systems are impaired due to previous treatments, and sometimes it is not possible to collect enough lymphocytes to generate CAR-T cells, or they are functionally abnormal.
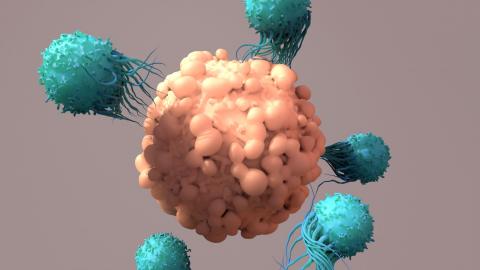
In an ongoing phase 1 clinical trial, Sham Mailankody et al. generated allogeneic CAR-T cells engineered to recognise the BCMA antigen, which is highly expressed on multiple myeloma cells, and combined them with an antibody that targets a cell surface glycoprotein called CD52, found on the patient's immune cells, to prevent them from rejecting the allogeneic CAR-T cells.
So far, 43 patients have been included in the trial and have been treated with increasing doses of allogeneic CAR-T cells. The authors show that the treatment is safe: 55.8% of patients develop a cytokine release syndrome with a single event of grade ≥ 3 (more severe forms) and neurotoxicity in 14%, with no events of grade ≥3 (below that described in similar studies with autologous cells). More frequent were infectious episodes, which occurred in 53.5% of patients and were grade ≥ 3 in 23.3%.
The overall response rate (the percentage of patients whose disease was reduced after treatment) was 55.8%, and among the 24 patients who received a high dose of CAR-T cells the response rate was 70.8%. This rate is slightly lower than that reported in other studies with autologous cells.
More patients and more follow-up will be needed to confirm these data, which preliminarily demonstrate the feasibility and safety of allogeneic CAR-T cell therapy for multiple myeloma.
Luis Álvarez - CART mieloma EN
Luis Álvarez-Vallina
Head of the Clinical Research Unit in Cancer Immunotherapy at CNIO-HMarBCN
It is a high-quality study. It is the first study using allogeneic anti-BCMA CAR-T cells (donor-derived and named ALLO-715) modified to express a second-generation CAR [chimeric antigen receptor] and edited with TALEN technology to inactivate the T cell-specific receptor alpha chain (TRAC) and CD52 genes, to reduce the risk of graft-versus-host disease (GVHD) and allow cell expansion and persistence of ALLO-715 in lymphodepleted patients with an anti-CD52 monoclonal antibody.
The key advantage of this type of allogeneic product is immediacy, as the time between patient recruitment, lymphodepletion and CAR-T cell infusion is only a few days, whereas in autologous CAR-T therapies [using the patient's own cells] the average time between apheresis and product availability is more than 30 days, which is too long for many refractory patients with no other therapeutic options.
Obviously this is a first study and it will be necessary to optimise multiple parameters such as dose, administration schedule, etc., but the results demonstrate the feasibility, safety and efficacy of this allogeneic CAR-T cell therapy in patients with multiple myeloma. Importantly, no cases of GVHD were documented and of the ten deaths that occurred during the course of the clinical trial, seven were related to tumour progression and three were due to severe infections (fungal pneumonia, adenoviral hepatitis and sepsis), which is related to the lymphodepletion strategy employed in this clinical trial.
Mailankody et al.
- Research article
- Peer reviewed
- Clinical trial
- People