Tiny organoids help repair liver damage in mice
Japanese scientists have developed tiny liver organoids from stem cells that, transplanted into mice, integrate with the original organ and help repair fibrotic lesions. This scar-like tissue damage is common to many liver diseases, such as fatty liver disease and cirrhosis. According to the authors, who publish their results in the journal Science Translational Medicine, such organoids could offer an alternative to liver transplants in the future.
Rafael Matesanz - organoides hígado EN
Rafael Matesanz
Creator and founder of the National Transplant Organisation.
The supply/demand disproportion is a universal phenomenon in all types of organ transplantation, but it is particularly distressing in the case of the liver because it is the most in demand after the kidney and because, unlike the kidney, it lacks alternatives such as dialysis and is therefore of a vital nature. For this reason, liver transplantation is currently the only solution for all types of end-stage liver disease.
The line of research proposed in this article could be revolutionary because, if it were fully implemented and applied in clinical practice, it would provide an effective treatment for liver fibrosis, which is a common final pathway for most liver diseases. It would therefore represent a solution for thousands of patients without access to transplantation.
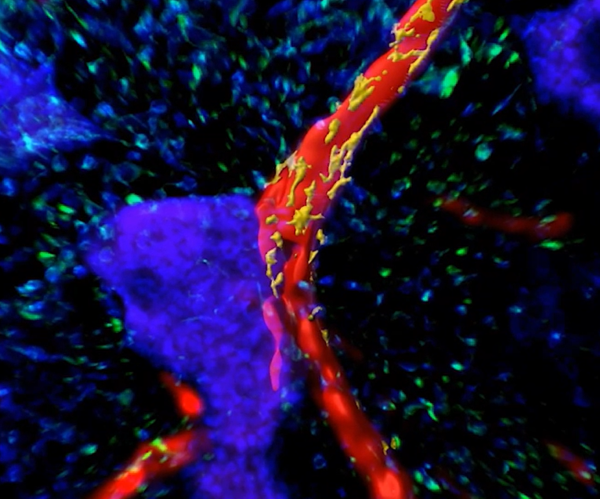
The method involves the use of pluripotent iPS cells in mice to create ‘liver buds’ which, once fused to form organoids, can be transplanted into the animal, leading to improved liver function in animals with chemically induced liver fibrosis. These liver organoids show a strong regenerative capacity, improve fibrosis through the action of macrophages and are able to develop their own structures such as bile ducts and blood vessels, as well as establish connections with the animal's original organ.
Although with the caution that comes with being a study in experimental animals and referring only to a specific form of experimental liver disease, this line of research, which follows previous work by the same team with a fairly solid track record, opens up a path with great possibilities in the search for alternatives to transplantation and thus to alleviate the shortage of organs.
240725 organoides ivan fernandez EN
Iván Fernández Vega
Full professor of Pathological Anatomy at the University of Oviedo, Scientific Director of the Principality of Asturias Biobank (BioPA) and Coordinator of the Organoid hub of the ISCIII Biomodels and Biobanks platform
The work is of high quality and very interesting from a scientific and social point of view. It uses a sound methodology, including well-designed experiments and adequate controls. It is a preclinical study conducted in immunodeficient rat and mouse animal models to investigate the therapeutic effect of transplantation of human induced pluripotent stem cell-derived liver organoids (hiPSC-LOs) on liver fibrosis through their immunomodulatory roles on macrophages (MFs). These organoids were created by fusing multiple liver buds derived from human induced pluripotent stem cells (hiPSC-LBs) and composed of different cell types, including hepatocytes (main cells of the liver), endothelial cells (which form blood vessels) and mesenchymal cells (which provide structural support). Part of this team of Japanese scientists led by Hideki Taniguchi (Nature, 2013) had already observed that hiPSC-LBs were able to create nascent and functional endothelial networks, which are essential for successful engraftment. Thus, being more ambitious, their intention in this paper was to scale up the process, to build hiPSC-LOs, and transplant them into models of chemically induced fibrosis to promote the generation of new liver tissue and restore function. The hiPSC-LOs have a more complex structure, perform key liver functions, and after transplantation, were able to create an adequate vasculature and bile duct system (at two weeks post-transplantation), and were comparable to the mid-gestation fetal liver in terms of histology and function.
Following the development of hiPSC-LOs and their histological, molecular (gene expression) and functional characterisation (superior compared to conventional hiPSC-LBs for ornithine transcarbamylase activity, human albumin secretion, transferrin secretion and ammonia clearance), they performed transplantation on the liver surface of preclinical liver fibrosis models, with successful formation of functional liver tissue on the liver surface. The work shows a significant improvement in survival rates, biochemical parameters, liver function and fibrosis reduction through a polarisation of macrophages towards the anti-inflammatory M2 phenotype in the liver microenvironment.
The study aligns well with existing evidence on the use of stem cells and organoids for tissue and organ regeneration. It provides significant novelty by demonstrating that hiPSC-LOs can not only integrate into the host liver and improve its function, but can also induce M2 macrophage polarisation, which is crucial for the reduction of fibrosis. This innovative approach offers a promising alternative to liver transplantation, especially given the global challenge of donor organ shortage.
The implications of this study are potentially revolutionary. If the results can be replicated and validated in clinical trials, hiPSC-LOs could offer a viable alternative to liver transplantation. This would not only ease the burden on the organ transplant waiting list, but also offer a less invasive and possibly safer solution for patients with end-stage liver disease.
Main limitations:
- Immunodeficient animal models: The use of immunodeficient animal models may limit the extrapolation of results to humans with a functional immune system. The immunological response in humans may differ significantly.
- Duration of study: Short-term observation may not reveal adverse effects or long-term complications, such as tumour formation or long-term graft integration.
- Differences between chemically induced fibrosis models and human diseases: Chemically induced liver fibrosis models do not fully recreate the human pathology of chronic liver diseases such as NASH (non-alcoholic steatohepatitis), which may limit the clinical relevance of the findings.
- Organoid heterogeneity: Variability in organoid composition and maturation may affect reproducibility and consistency of results, which is a common limitation of organoid studies.
- Scalability and mass production: Large-scale production of liver organoids with consistent characteristics is challenging, which could limit the practical and clinical applicability of the technology.
-
Safety and Preclinical Assessments: Although no tumours were detected in the study in the short-term, more comprehensive long-term safety assessments are required, including toxicity, tumourigenicity and pharmacokinetic studies.
Finally, it should be emphasised that the study was neither randomised nor double-blinded, which could reduce its internal validity by generating treatment allocation biases, as well as observer biases that could influence data evaluation and analysis, among others.
In conclusion, the article highlights important contributions to the field of regenerative medicine and proposes an innovative therapeutic alternative (liver organoid transplantation on the liver surface) as a measure to improve liver function and decrease fibrosis, improving survival rates in the animal models used. This opens a path of hope for the treatment of multiple liver pathologies, especially those whose common final pathway is liver cirrhosis with severe liver failure.
Tadokoro et al.
- Research article
- Peer reviewed
- Animals



