Center for Applied Medical Research (CIMA)
If you are the contact person for this centre and you wish to make any changes, please contact us.
Researcher in the Gene Therapy and Regulation of Gene Expression Programme and Director of Innovation and Transfer at Cima University of Navarra
Professor of Immunology at the University of Navarra, CIMA researcher and co-director of the Department of Immunology and Immunotherapy at the Clínica Universidad de Navarra.
Senior Researcher of the Gene Therapy in Neurodegenerative Diseases Programme at the Centre for Applied Medical Research (CIMA), University of Navarra
Researcher in the Solid Tumours Programme at CIMA and the Clínica Universidad de Navarra
Researcher of the Gene Therapy and Regulation of Gene Expression Programme at Cima (Centre for Applied Medical Research) University of Navarra

A phase 3 clinical trial conducted in China tested 210 patients with advanced non-small cell lung cancer—the most common type—to see whether the time of day when immunotherapy and chemotherapy were administered influenced their effectiveness. The data indicate that, on average, those who received therapy after 3 p.m. did not see their cancer worsen for 5.4 months. In contrast, those who received it before that time did not see their cancer worsen for an average of 11.7 months, almost twice as long. Overall, response rates were 56.2% and 69.5%, respectively. The results, published in Nature Medicine, suggest that scheduling therapy early in the day may offer a simple and cost-free way to improve treatment efficacy.

An international team with Spanish participation has analyzed data from more than 500,000 people and found a link between digestive disorders such as colitis, gastritis, esophagitis, or functional bowel disorders and an increased risk of developing Alzheimer's and Parkinson's diseases. According to the researchers, who published their findings in the journal Science Advances, “this effort sheds light on the interaction between factors involved in the gut-brain axis and opens avenues for targeted treatment and early diagnosis.”
Certain immunotherapy treatments for cancer work by releasing the brakes on our defences. However, their response varies and is not uniform in all patients. A team in the United States has now published a study in Nature according to which certain autoantibodies present in patients could improve the efficacy of the therapy, which would explain some of this variability and could be used to design future complementary treatments.
A phase 1 clinical trial has tested the safety and preliminary efficacy of a new form of CAR-T cell therapy - which they call “armed” - in patients with lymphoma. The novelty consists of adding another gene to help increase response. Of the 21 patients treated, all resistant to multiple lines of treatment including approved CAR-T therapies in 20 of them, 81% showed a response and 52% went on to achieve complete remission without significantly greater side effects than with the standard option. The results are published in the journal NEJM.

In 2050 there will be 25.2 million people with Parkinson's disease worldwide, which represents an increase of 112% from 2021, largely due to the ageing of the population, according to a modelling study published by The BMJ. The number of people living with this disease – prevalence across all ages – per 100,000 inhabitants is expected to increase by 76% – and by 55% when age differences are corrected.

An international team has found that aspirin is capable of reducing the appearance of metastasis in mice, by enabling the activation of T lymphocytes capable of recognising tumour cells. The research showed that several different mouse cancer models — including breast cancer, colon cancer and melanoma — treated with aspirin showed a lower rate of metastasis in other organs, such as the lungs and liver, compared to untreated mice. According to the authors, who publish the results in the journal Nature, ‘the finding paves the way for the use of more effective anti-metastatic immunotherapies’.

A team of US researchers has followed some patients treated with CAR-T therapies in a small clinical trial conducted between 2004 and 2009 to treat children with neuroblastoma, a nerve cell tumor that can have a poor prognosis. At least one of them, a woman who was treated with CAR-T as a child, remains in remission 18 years later, the longest duration of such therapy described to date. The results are published in the journal Nature Medicine.

CAR-T cell-based treatments have been successful against some blood tumours, but are much less effective for solid tumours. A phase 1 clinical trial has tested their use in 11 children and young adults with diffuse midline glioma, a tumour of the nervous system that is considered incurable. The results, published in the journal Nature, indicate that the treatment improved functional status in nine of the 11 patients. One of the four who showed a strong response is still healthy four years later.

The regulatory agencies for medicines in the United States and Europe have issued statements informing about a possible risk of developing certain types of tumors following CAR-T cell immunotherapy treatment. What do we know so far? What is the real risk? Does the benefit-risk balance still hold? Has anything changed after these alerts? We answer these questions with expert opinions and the data currently available.
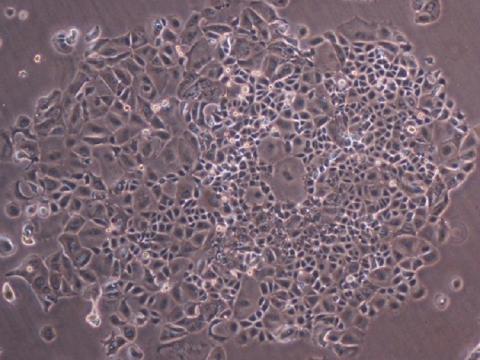
CAR-T cell therapies may, in some cases, produce tumours secondary to treatment. A few months ago, the US Food and Drug Administration (FDA) said it was assessing this risk. Now, a study conducted at Stanford University Medical Center (USA) has tracked 724 patients who received this type of treatment since 2016. Of these, 14 developed another blood tumour, but only one was a T-cell lymphoma that could be a direct consequence of the therapy. Further analysis ruled out this link. The results are published in the journal NEJM.