CAR-T therapy tested to treat childhood brain tumours considered incurable
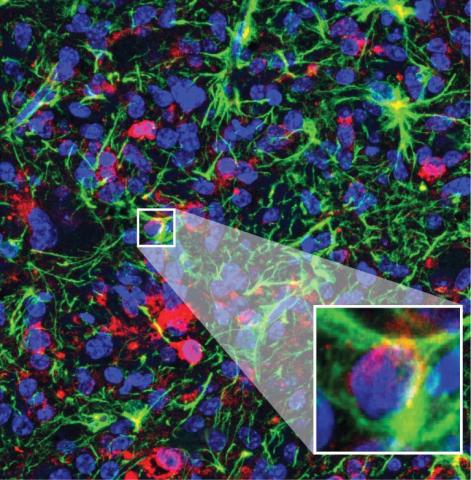
CAR-T cell-based treatments have been successful against some blood tumours, but are much less effective for solid tumours. A phase 1 clinical trial has tested their use in 11 children and young adults with diffuse midline glioma, a tumour of the nervous system that is considered incurable. The results, published in the journal Nature, indicate that the treatment improved functional status in nine of the 11 patients. One of the four who showed a strong response is still healthy four years later.

Manel Juan - CAR-T fase 1 niños EN
Manel Juan
Head of the Immunology Service
This is a very important study in a disease that has a terrible prognosis (Diffuse Intrinsic Pontine Pontine Glioma, known in the field as DIPG). With only 11 patients in a phase 1 trial to demonstrate safety, it provides enough response data (9 of 11 patients) to be able to say that we are in a preliminary but crucial year for the treatment of nervous system tumours with CAR-T therapy to be approved for systematic use, because unlike other solid tumours where the results are usually clearly insufficient for the CAR-Ts studied, in brain tumours several very clear and more than promising proposals have been published since February 2024.
In addition, this case of the 9 patients with responses includes a young adolescent-adult who has been without detectable disease for 4 years. The study is technically flawless for this safety study, and very promising in suggesting efficacy.
The study reinforces the idea that brain tumours are likely to be treatable by CAR-T. The main (and initial) implication is in the case of DIPGs, where there is really no chance of 2-year survival in children. With this study, there is clear hope for effective treatment for those who do not have it. Other work in the field (mainly in glioblastoma multiforme) published in 2024 (and some earlier) shows that CAR-T can and will be effective for solid tumours (non-hematological, as in the case of haematological tumours, almost 40,000 patients worldwide have already received this last-line treatment, with data that at all levels are considered spectacular).
Other implications beyond brain tumours such as DIPG are that other solid tumours are approachable, although possibly needing to incorporate improvements in the basic conventional procedure. In this regard, data related to local reinfusion in brain compartments indicate that enhancing CAR-T lymphocyte localisation is relevant. Finally, it is also confirmed that GD2 [antigen] may be a good target in these tumours, a controversial concept as many adverse effects have been found in the use of this target with monoclonal antibodies. It is clear from the work that we should not infer results from products with the same target if the effector media are different.
The results also imply that the route of administration (directly into the central nervous system) is more convenient, less toxic and potentially more effective. Finally, there is the fact that it opens up the possibility of ‘chronifying’ a currently incurable disease (an important concept in immunotherapy and one that in some ways distinguishes it from radiotherapy or chemotherapy, as immunotherapy treatment can endure and integrate into the body itself as a ‘living drug’, whereas radiotherapy and chemotherapy only act as long as they are applied).
Of course, as most of the positive results with CAR-T open the door to explore new CAR-T and immunotherapy combinations to try to anticipate the mechanisms of tumour immunoediting and escape (also very relevant in neurological tumours).
It is worth remembering that treatment with anti-GD2 CAR-T was shown in another Italian study published in NEJM to be effective in neuroblastoma, another neurological tumour. Both reinforce the relevance of the safety and potential efficacy of these CAR-Ts with this target, although other targets (in combination) will surely be essential to ensure that these tumours have real therapeutic options.
The main limitation of the study has to do with the low number of cases treated and the fact that only one patient seems to achieve a complete response (with ‘only’ 4 years of follow-up, but in this disease this is much more than any other treatment has achieved so far). This is an intrinsic limitation that in no way detracts from the quality of the work, which does not claim to be definitive or conclusive.
Conflict of interest: ‘I do not have any conflict arising from economic impact on me personally. The main conflict of interest is my personal bias in considering CAR-Ts as the main option for the medium-term therapeutic future in oncology. We are also in scientific contact with Dr Crystal Mackall [one of the authors of the study] and Stanford University. We hope to have future collaborations with them. On the other hand, there is some conflict because during 2025 we hope to start with Dr Andrés Morales de la Madrid at Hospital Sant Joan de Déu a CAR-T proposal in DIPG patients with another target (anti-IL13Ra2), which has also shown efficacy'.
Marta Alonso - CAR-T fase 1 niños EN
Marta María Alonso Roldán
Researcher in the Solid Tumours Programme at CIMA and the Clínica Universidad de Navarra
It is an important study for an indication for which, to date, there is no cure. Work like this, which is different from continuing to test small molecules or conventional chemotherapy, is very relevant.
It is a quality study. Stanford is a leading centre and the study is done with all the necessary quality parameters. They are not talking about an isolated case but about a regulated study that has passed several filters.
It is a different approach based on cell therapy and CARs, which have given very good results in haematological tumours but whose efficacy in solid tumours has yet to be demonstrated.
This is a phase I trial that shows that it is possible to approach this type of study in this type of patient. It also shows that we do not have to be afraid of toxicities if we have ways to manage them and they are accompanied by clinical improvement. Finally, the study indicates some efficacy, which opens the door to future trials and raises the need for combinations for this type of tumour.
The biggest limitation of this study is that patients were highly selected to have good performance status and tumours of adequate size. It will be interesting to see what happens with a more heterogeneous patient population.
Melero - CAR-T ensayo fase 1 niños EN
Ignacio Melero
Professor of Immunology at the University of Navarra, CIMA researcher and co-director of the Department of Immunology and Immunotherapy at the Clínica Universidad de Navarra.
The most interesting aspect of the study is that intracavitary locoregional delivery is the way forward. This intracavitary or intratumoral route of administration can optimise CAR-T cell performance against solid tumours with maximum exposure. In the case of intracranial administration, it must be taken into account that inflammation of the tumour (tumouritis) will occur and that there are risks of intracranial hypertension requiring intensive monitoring and treatment if this adverse effect occurs. On the other hand, other side effects such as systemic cytokine release syndromes (cytokine storms) do not occur via this route.
Other groups such as Marcela Maus' group have used the intracranial route in patients with glioblastoma multiforme with encouraging results. We have recently published a review on the local approach in the use of adoptive cell therapy that may be useful.
Vallina - CAR-T fase 1 niños EN
Luis Álvarez-Vallina
Head of the Clinical Research Unit in Cancer Immunotherapy at CNIO-HMarBCN
The work is of high quality, with a careful experimental design and based on very solid preclinical results from the promoter group. Important data on the cell production process as well as on the toxicity and safety profile after intravenous and intracerebral infusion are analysed and obtained.
The study reinforces previously published data on the enormous potential of adoptive cell therapies based on ‘T-lymphocyte redirection’, in particular CAR-T cells, for the treatment of brain tumours. The results represent a real ‘accolade’ for this immunotherapy in terms of safety and efficacy, as it documents a case of complete remission in a patient with diffuse midline glioma, which is an incurable pathology. This study, along with others previously published, demonstrates that this type of adoptive cellular immunotherapies will become the gold standard treatment for brain tumours in the short term, and paves the way for future evolutions of this type of therapy to improve its efficacy.
[In terms of limitations] The observation period in the regressed patient is still too short to draw definitive conclusions. In addition, it is essential to deepen the immunological aspects of the response to accurately determine the persistence and location of CAR-T cells, as well as the type or nature of the induced immune response. This will be key in order to be able to implement therapy and increase response rates.
Monje et al.
- Research article
- Peer reviewed
- Clinical trial
- People