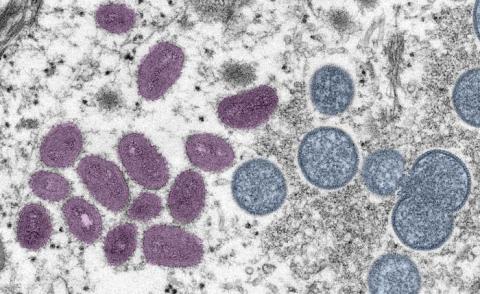
On 7 May 2022, the UK announced that it had detected a case of monkeypox in a person who had recently travelled to Nigeria. This was not the first time the disease had been found outside Africa, but the discovery of more cases in the following weeks, both inside and outside the country, confirmed that this was an unprecedented outbreak.
For the time being, the WHO has not declared the current outbreak of monkeypox a "public health emergency of international concern". However, the number of confirmed cases is close to 3,500 in 50 countries.
Stigmatisation, discrimination and xenophobia are a constant in the history of infectious diseases. During the onset of the covid-19 epidemic, Chinese - and Italian - citizens suffered the consequences of belonging to the countries that were affected first, before the coronavirus spread across the globe.
Similarly, the vast majority of monkeypox cases have been detected in gay, bisexual and men who have sex with men (MSM). This raised fears of repeating the mistakes made during the HIV pandemic, while recalling the lessons learned then.
For how do you communicate the risks of an outbreak when the most affected population is also susceptible to being singled out?
The right thing to do is to inform
María del Carmen Climent, a researcher at the Winton Centre, University of Cambridge (UK), and member of the SMC Spain advisory committee, explains that "it will always be appropriate to report risk factors for any disease, including having homosexual relations if there is evidence to that effect". The important thing, he says, is "to do it in a balanced way, without prejudice and without yellow headlines".
Different countries have opted for different communication strategies to reach the most affected groups. The UK Health Safety Agency (UKHSA) produced a video in which an epidemiologist from the LGTBI+ community mentioned that most of the cases had occurred in gay and bisexual men and reported the symptoms to have a "happy, safe and healthy" Pride.
WATCH ? @teozka gives advice on having a happy, safe and healthy #Pride to everyone celebrating & what people should look out for with #Monkeypox.
— UK Health Security Agency (@UKHSA) June 1, 2022
Get the latest updates ?
The Spanish Ministry of Health, on the other hand, resorted to a more general campaign reminding people that sexual relations, for both men and women and regardless of sexual orientation, are risky activities. This campaign has been advertised on sites such as dating apps in an attempt to reach the population of interest.
? En 2022 #FiestaSaludable
— Ministerio de Sanidad (@sanidadgob) June 21, 2022
?#Monkeypox se transmite por:
✔️Contacto estrecho
✔️Relaciones sexuales, en hombres y en mujeres, independientemente de la orientación sexual
?Sigue las medidas de higiene y obsérvate ??
?Si tienes síntomas, acude al Centro de Salud o Centro ITS pic.twitter.com/0tpXOSpAgP
A piece of advice: anticipate prejudice
Climent recommends "anticipating existing prejudice and overcoming it or clarifying it with evidence". For example, clarifying misconceptions such as that homosexual men are more at risk of contracting and transmitting the disease or that heterosexual men are not at risk. "You can never conclude something about an individual from population data," he says.
Beware of confirmation bias
The so-called "confirmation bias" is a problem that can occur in outbreaks such as the current one, warns Fisabio preventivist Salvador Peiró in an article published in The Conversation. This occurs "when detection is differential between population groups because their exposure or risk is different".
In other words, men who have sex with men are more likely to seek medical attention for these symptoms, so more cases are detected among them, so health workers will look more for the disease in them... and the cycle repeats itself. This can cause an outbreak to spread under the radar as it did at the beginning of the covid-19 pandemic, when only those who had recently visited countries such as China and Italy were considered at risk.
No simple answer
In 2020, a team of risk communication researchers looked at how to effectively communicate about diseases such as HIV. The problem, they argued, is that where there is a health "disparity", messages are targeted at high-risk subgroups. The aim is to achieve a number of desired effects (such as an increase in their perception of risk), but undesirable ones (such as stereotyping and mistrust) may be achieved along the way.
"There is not yet a clear evidence-based approach to communicating about health disparities while avoiding potential unintended effects," they concluded. While noting that the available literature was sparse in the context of HIV, they did make a number of recommendations: for example, evoking positive emotions that motivate action, promoting transparency and credibility of information, and using images that avoid reinforcing stereotypes.