Bladder cancer patients with colour vision deficiency have lower survival rates than those without this visual impairment
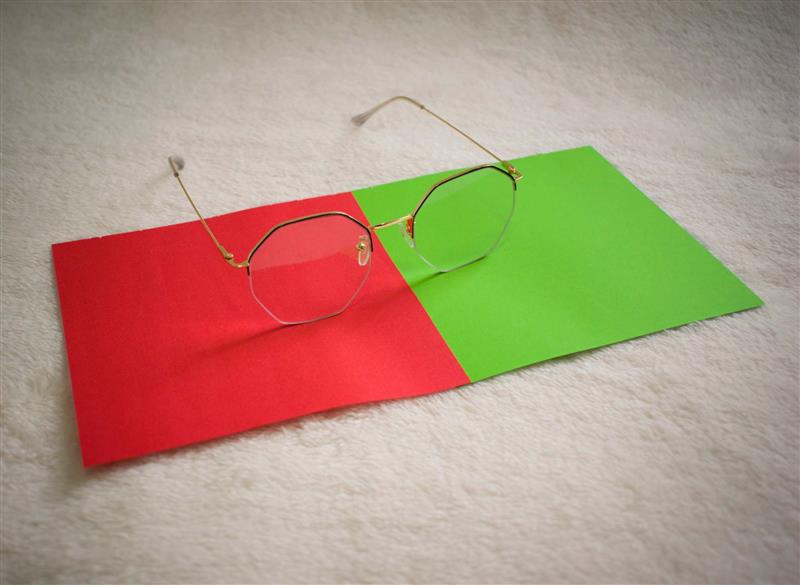
People with colour vision deficiency and bladder cancer have lower survival rates than patients with the same cancer who have not been diagnosed with this visual condition, according to an analysis of medical records between 2004 and 2025 comparing a group of 135 people with both diagnoses and another group of 135 with bladder cancer without visual impairment. In a study published in Nature Health, the authors suggest that this difference could be due to these patients not detecting the presence of blood in their urine, which delays the seeking of medical care and cancer diagnosis.
260115 cancer vejiga félix EN
Félix Guerrero-Ramos
Coordinator of the Uroncology Unit at the 12 de Octubre University Hospital in Madrid, and medical doctor at ROC Clinic and HM Hospitals
This study puts forward a simple but relevant idea: some people may take longer to detect cancer simply because they do not perceive one of its main symptoms well. Specifically, the authors analyse whether patients with colour blindness have a worse prognosis when they develop bladder cancer, as they may not be able to identify blood in their urine, which is often the first sign of the disease.
Based on the analysis of a large database of electronic medical records, the study shows that patients with bladder cancer and colour vision deficiency have lower survival rates and a higher risk of long-term mortality than those without this visual impairment. The explanation is plausible: bladder cancer usually begins with painless haematuria, i.e., visible blood in the urine without other symptoms. If a person cannot distinguish the colour red well, they may not notice this warning sign and delay consulting their doctor.
It is particularly interesting that this effect is not observed in colorectal cancer. In that case, although blood may also appear in the stool, there are well-established screening programmes and other symptoms, such as abdominal pain or changes in bowel habits, that can alert the patient. This reinforces the idea that the problem is not the cancer itself, but the difficulty in recognising a key symptom when detection depends almost exclusively on visual observation.
That said, it is important to be very cautious when interpreting the results. This is a retrospective study, based on clinical records, with significant limitations. Many people with colour blindness are not officially diagnosed, so the actual number of people affected is likely to be higher. Furthermore, the study does not provide detailed information on the stage of the tumour at the time of diagnosis, making it impossible to confirm directly that the poorer survival rate is due to later diagnosis.
In clinical practice, these data do not imply that bladder cancer screening recommendations should be changed immediately. However, they do call for greater awareness. In people with risk factors (such as being over 70 years of age, using or having used tobacco, and working with industrial paints), knowing about the existence of a colour perception deficit can help to provide them with recommendations on how to better interpret symptoms (even with the collaboration of a family member who periodically checks the subject's urine). In this sense, the study opens up a new line of research on how certain sensory limitations can influence the early diagnosis of cancer and, potentially, its prognosis.
Conflicts of interest:
- Research support/PI: Johnson & Johnson, Pfizer, Taris, BMS, Roche, Seagen, AstraZeneca, Combat Medical, Cepheid, Fidia, Astellas, UroGen, MSD, enGene, Tyra Bio.
- Employee: SERMAS (Servicio Madrileño de Salud).
- Consultant: Johnson & Johnson, Pfizer, Merck, Roche, Taris, Combat Medical, AstraZeneca, MSD, BMS, enGene, Nanobots Therapeutics, Gebro, Photocure.
- Stockholder: CG Oncology, Johnson & Johnson, Pfizer, Danae Urogenomics.
- Speaker bureau: Nucleix, MSD, Pfizer, Merck, BMS, AstraZeneca, Palex, Combat Medical, Johnson & Johnson, Recordati, Gebro.
- Travel: Pfizer, Recordati, Ipsen, Combat Medical, Alter, Salvat, Nucleix, AstraZeneca, Fidia, Johnson & Johnson.
- Scientific advisory board: AstraZeneca, BMS, Combat Medical, Johnson & Johnson, Nucleix, Pfizer, Taris, Roche, MSD, enGene.
- Manuscript support: Pfizer, Janssen, Combat Medical, AstraZeneca, Johnson & Johnson, BMS, Gebro.
- Others: Co-founder of Danae Urogenomics.
260115 cáncer vejiga leticia EN
Leticia Álvaro Llorente
Permanent lecturer, Faculty of Psychology, Daltonism and Design Research Group
Julio Lillo Jover
Professor of Ergonomics, Faculty of Psychology, Colour Blindness and Design Research Group
Humberto Moreira Villegas
Professor in the Psychology Division
Is the study based on sound data and methods?
"Yes. On the one hand, the data comes from the TriNetX database, which includes medical records from 275 million anonymous patients, backed by standardised procedures. On the other hand, the study presents a retrospective cohort design, with a large sample of 135 controls and 322 patients with colour vision deficiencies (135 diagnosed with bladder cancer and 187 diagnosed with colorectal cancer)."
How does it fit in with previous work? What new information does it provide?
"Previous studies had already pointed out that colour blindness can make it difficult to visually detect blood, a key symptom of some cancers. The main novelty of this work is that it links colour vision deficiencies with worse survival outcomes in bladder cancer, but not in colorectal cancer".
Are there any important limitations to consider?
"Yes. This type of study does not allow us to infer direct causality, only an association between two variables, in this case bladder cancer and colour vision deficiencies. In addition, colour vision deficiencies are often underdiagnosed, so there could be classification errors in the control group. These errors could have reduced the association with bladder cancer, but they could also have prevented the association with colorectal cancer from being detected."
How relevant is this study in practice/clinical settings? What recommendations can we make based on it?
"The study suggests that colour blindness could be an indirect risk factor for late diagnosis of bladder cancer, as one of the first signs of this disease is the presence of blood in the urine, which people with colour vision deficiencies may not easily detect. In practice, it reinforces the importance of not relying solely on patient observation and of considering more proactive screening or follow-up strategies, something that is highlighted by the results of this study in relation to people with colour blindness, but which would also benefit patients with normal vision. Finally, it emphasises the need to raise awareness among healthcare professionals and patients about this possible diagnostic bias."
Mustafa Fattah et al.
- Research article
- Peer reviewed
- Observational study
- People