Administering immunotherapy and chemotherapy in the morning could improve their effectiveness against lung cancer
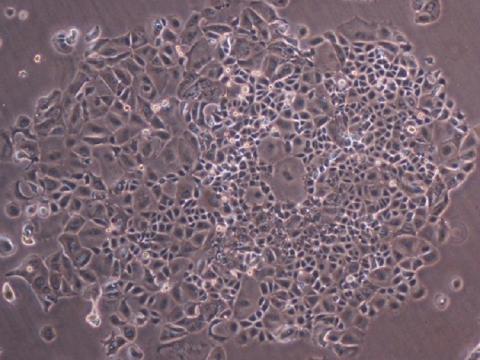
A phase 3 clinical trial conducted in China tested 210 patients with advanced non-small cell lung cancer—the most common type—to see whether the time of day when immunotherapy and chemotherapy were administered influenced their effectiveness. The data indicate that, on average, those who received therapy after 3 p.m. did not see their cancer worsen for 5.4 months. In contrast, those who received it before that time did not see their cancer worsen for an average of 11.7 months, almost twice as long. Overall, response rates were 56.2% and 69.5%, respectively. The results, published in Nature Medicine, suggest that scheduling therapy early in the day may offer a simple and cost-free way to improve treatment efficacy.

María Casanova - inmuno hora EN
María Casanova
Head of the Cancer Immunity Group at the CNIO
This article marks a turning point, as it provides the first evidence that administering immunotherapy in the afternoon has a modulating effect on the adaptive immune system, specifically on T cells.
A non-causal association was already known; now that causality has been established in this study. The immediate implications are to move a large part of immunotherapy treatments to the afternoon. This study establishes this connection, but it remains to be explored whether it is solely the administration of the drug in the morning or whether there are other determinants in this specific cohort of patients that also contribute to the response."
Are there any important limitations to consider?
‘Yes, the number of patients (210), as well as the extrapolation to other types of tumours. It is an extremely provocative study, which will undoubtedly motivate new trials along these lines to identify whether we can establish biomarkers to know which patients can benefit from the timing of immunotherapy administration.’,
Amancio Carnero - inmuno hora EN
Amancio Carnero Moya
Principal investigator of the Molecular Biology of Cancer group at the Institute of Biomedicine of Seville (IBIS)
It is a good article published in one of the best journals in the field. The article presents part of a phase 3 randomised trial with 210 participants and suggests that scheduling therapy early in the day may offer a simple and inexpensive way to improve standard care.
Circadian rhythms, the internal 24-hour clock, are known to affect immune cell behaviour and response to treatment, especially with therapies that require the immune system to act, such as immunotherapy. Previous retrospective studies on cancers suggest that administering immunotherapy (checkpoint inhibitors) early in the day may be more effective. However, no prospective randomised controlled trials have been conducted to validate these preliminary findings.
The authors conducted a prospective, randomised phase 3 study involving 210 patients with advanced non-small cell lung cancer who had not previously been treated. Patients were assigned to receive immunochemotherapy before 15:00 (early group) or at 15:00 or later (late group) during the first four cycles of treatment. After a follow-up of approximately 28.7 months, the late group showed no worsening of cancer (progression-free survival, PFS) for an average of 5.7 months, while the early group remained without worsening cancer (PFS) for almost twice as long, an average of 11.3 months. The median overall survival was 28 months in the early group and 16.8 months in the late group. Treatment response rates were also higher in the early group than in the late group, and no significant differences in immune-related adverse events were observed. In other words, treatment in the morning appears to be more effective (almost twice as effective) than treatment in the afternoon.
In principle, this is a well-controlled study with clear results based on the data provided.
It was known that circadian rhythms affect immune cell behaviour and response to treatment. Previous retrospective studies on cancers such as kidney cancer and malignant melanoma have suggested that administering immunotherapy (checkpoint inhibitors) early in the day may be more effective. However, no prospective randomised controlled trials have been conducted to validate these preliminary findings. The result of this trial, as the authors say, opens the door (if these results are validated elsewhere/in other hospitals) to increasing the efficacy of immunotherapy in a simple way, simply by changing the time of administration of the therapy.
The authors observed more CD8⁺ T cells circulating in the blood (a type of immune cell) and a higher proportion of activated versus exhausted CD8⁺ T cells in the early treatment group than in the late treatment group, which could explain the greater efficacy of the therapy in this group. Although these are preliminary results and need to be confirmed and supplemented with the correct mechanism of action, it could explain the results, since, for example, rest or the body's metabolic state due to the circadian clock in the early hours could justify a better immune component that would help in treatment processes with immunotherapies.
The most important limitations are, for example, that the patient population was focused exclusively on China, requiring validation in other countries and contexts to extend the findings to patients in general. In addition, more research is needed to present overall survival data and, above all, the mechanism of how and why this phenomenon occurs, or factors that may interfere with it.
Ignacio Melero - inmuno hora EN
Ignacio Melero
Professor of Immunology at the University of Navarra, CIMA researcher and co-director of the Department of Immunology and Immunotherapy at the Clínica Universidad de Navarra.
These results are surprising and difficult to understand, given that the half-life of the agents is weeks, and yet the time of administration radically influences the results. I am very pleased that our infusions in my unit are almost always in the morning. These results provide sufficient evidence for this to become routine from now on.
Ramón Salazar - hora inmunoterapia EN
Ramón Salazar
Head of Medical Oncology at the Catalan Institute of Oncology (ICO), head of the Colorectal Cancer Research Group, Oncobell programme (IDIBELL) and associate professor of Medicine at the University of Barcelona
“Overall, this is a randomised phase 3 trial that addresses a very specific clinical question—whether the time of administration influences the efficacy of immunochemotherapy—and does so with a prospective design and an independent, blinded committee to evaluate responses and progression, which reinforces the quality of the data.
The results are very striking: administration before 3 p.m. is associated with statistically significant improvement in both PFS and OS, with HRs of 0.40, which is associated with a clinically relevant effect size, more than sufficient for the approval of new drugs, for example."
How does this fit with the evidence already known, and what implications could it have? Is such a difference in response plausible based solely on the time of administration?
"It fits with previous, mainly retrospective literature and a meta-analysis that already suggested better results when PD-1/PD-L1 inhibitors are administered earlier in the day; the relevant contribution here is that it confirms this in a phase 3 randomised trial in advanced lung cancer.
From a biological point of view, it is plausible that the circadian clock modulates immune function; the study itself shows differences in peripheral blood consistent with greater cytotoxic “tone” (e.g., increased CD8+ and a more favourable balance between activation and exhaustion) in the early-treated group.
If confirmed in other contexts, the practical implication is enormous because changing the time of infusion would be a simple and cost-free intervention, potentially capable of improving outcomes with the same treatment".
Are there any important limitations to consider?
"The effect size is too large to depend “only” on the time, so the prudent interpretation is that the trial provides a very strong signal but needs replication and analysis of possible organisational bias factors or actual exposure to the intervention.
It is a single-centre study (China) with a highly male population (≈90% men), which means that generalisation to other healthcare systems and populations needs to be confirmed.
Randomisation was without stratification and the trial is open-label for logistical reasons; although progression was assessed by an independent committee, the absence of blinding may influence clinical decisions or indirect exposures. Some of the biological data (activated/exhausted subpopulations) comes from small subsamples and is exploratory, with comparisons not adjusted for multiplicity; this supports plausibility but is not definitive mechanistic evidence.
In summary, this work suggests that something as routine as scheduling immunotherapy in the morning could have a relevant clinical impact on advanced lung cancer, but the magnitude of the benefit requires multicentre confirmation before changing standards across the board".
Antonia - Crono
Antonia Tomás Loba
Head of the Circadian Rhythm and Cancer group at the Pascual Parrilla Murcian Institute of Biosanitary Research and Vice Dean of the Faculty of Biology at the University of Murcia
The article presents a retrospective study of patients with advanced non-small cell lung cancer (NSCLC). The randomized clinical trial was conducted with 210 patients and presented two therapeutic approaches:
- 105 patients treated before 3 pm.
- 105 patients treated after 3 pm.
The data show that patients treated in the first time slot, in the morning, had greater tumor-free survival and overall survival than those treated in the afternoon, with similar toxicity.
The work is of high quality and is led by leading scientists in the field. This includes oncologists specializing in chronotherapy, such as Dr. Zhang (Central South University, China), an expert in lung cancer; and Dr. Francis Levi (University of Paris-Saclay), whom we could call one of the pioneers of chronotherapy. and Dr. Scheiermann (University of Geneva), whose contributions to the field focus on describing the molecular mechanisms behind the effect of time of day on immunotherapy administration in preclinical models.
Chronotherapy is not a new therapeutic approach. The pioneering studies of Dr. Halberg in the 1970s and later Dr. Levi already demonstrated that drugs do not act the same way at every time of day. This evidence has taken a long time to gain traction in clinical practice and even in basic science, as chronotherapy has been viewed with some skepticism. We are currently experiencing a golden age in chronobiology and chronotherapy. There is increasing data that strongly supports Heraclitus's saying: "A man does not step into the same river twice," meaning that we are not the same at every time of day.
If we had the ability to take a molecular snapshot (and now we can, thanks to powerful 'omics' technologies) of each of us at different times of day, we would see that we are very different. This means that within a specific time window, we are more efficient at performing certain biological functions. If we translate this to clinical practice, the diagnosis of diseases is also dependent on the time of day. We are witnessing that the treatment of diseases is as well.
Not only is such a difference in response based on the time of day plausible, but it also has an indisputable biological basis. In the case of the study mentioned here, it refers to the efficacy of two of the administered drugs, which are immunotherapeutic agents (sintilimab and pembrozilumab), but this can be extended to other chemotherapeutic agents whose targets may be expressed at a specific time of day, according to molecular mechanisms that occur at a particular time. Dr. Scheiermann, the author of the study, previously described in preclinical models that anti-PD-1 therapy was more effective in the active phase, since ICAM-1, a molecule that helps the drug penetrate tumors, is expressed more during this phase. In other words, there is a time of day when the drug is more likely to reach the tumor because there is an agent that picks it up from the bloodstream and introduces it into the tissue—it's that simple.
We are beings of time, and therefore, not everything happens at any time of day.
This work helps to solidify an idea that is, a priori, easy to implement: that the same drug can be more effective because its activity is enhanced and/or its toxicity reduced if administered at a specific time of day. Of course, each drug and its optimal time of administration will have to be tested on specific tumors and their stages. There is still much to be done, but the window to understanding the molecular mechanisms and their testing and application in the clinic is now a reality.
[Regarding potential limitations] As I mentioned before, much remains to be studied and understood, considering that new studies must be conducted depending on the drug, tumor type, and stage. This study focuses on advanced-stage NSCLC, where several drugs, including sintilimab and pembrozilumab (immunotherapeutic agents), are used for chronomodulation. Therefore, the results cannot be extrapolated to other tumor environments, as each drug and each tumor presents a different chronobiological scenario. Furthermore, data reveal a different response to chronodirected treatments depending on sex, especially in hormone-dependent tumors. The gender dimension must also be considered in therapy, as must the patients' age.
Retrospective trials are necessary, and more hospitals should participate in these types of studies, but an understanding of the molecular mechanisms underlying the outcome is also needed.
Finally, hospitals must be prepared to administer chrono-directed therapy. This will require hospital management to integrate the concept of circadian medicine into their daily practice and implement it in the diagnosis and treatment of diseases.
Huang et al.
- Research article
- Peer reviewed
- Randomized
- Clinical trial
- People