High-risk Human Papillomavirus (HPV) genotypes linked to reduced male fertility
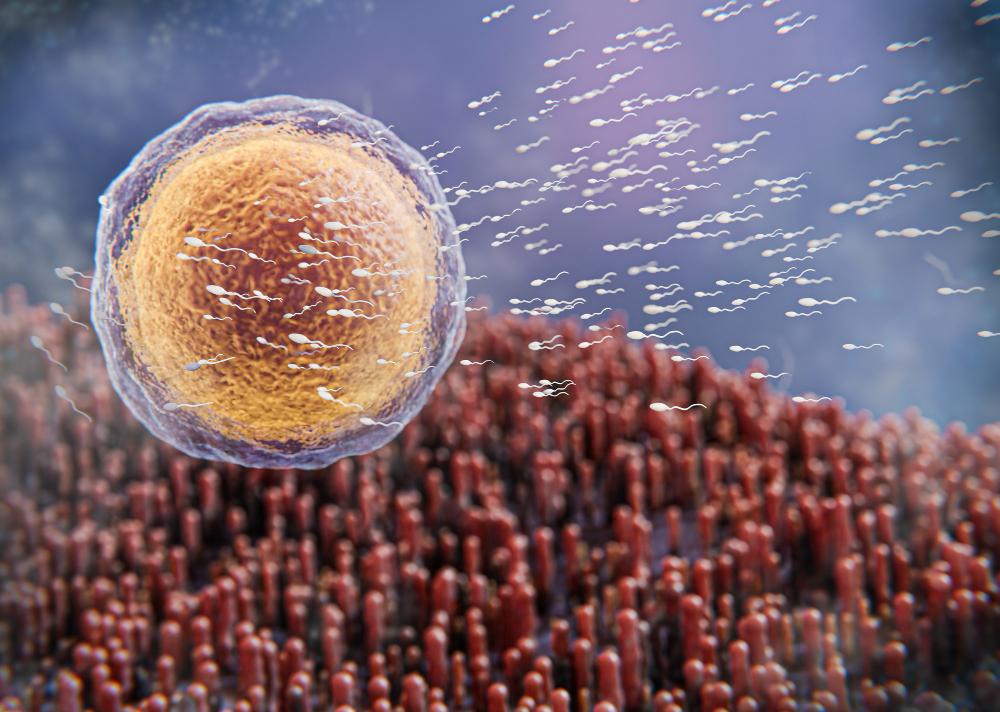
The sperm of men infected with high-risk genotypes of the human papillomavirus (HPV) suffers more damage from oxidative stress and has a weaker immune response, which can lead to reduced fertility. This is one of the conclusions of a study published in the journal Frontiers in Cellular and Infection Microbiology. The research compared the semen of 20 adults infected with high-risk genotypes, seven infected with low-risk genotypes, and 43 adults without infections.
Yolanda Cabello - Fertilidad varones y VPH EN
Yolanda Cabello
Independent clinical embryologist and consultant in assisted reproduction and lecturer on the Master's Degree in Health and Clinical Management at the International University of Valencia
Human papillomavirus (HPV) infection is considered one of the most common sexually transmitted infections worldwide. It is estimated that up to 80% of the sexually active population (both men and women) may come into contact with the virus at some point in their lives, even if they are not aware of it.
This widespread prevalence has made it difficult to establish a connection with infertility until in-depth studies on this matter have been conducted, most of which have focused on women. Traditionally, women are screened for the presence of the virus during annual gynecological check-ups (through cytology, and later specifically for HPV). The reason is that there are different genotypes of this virus, categorized as low or high risk, with two of the latter being responsible for cervical cancer. Recently, there has been a notable increase in penile, rectal, or even oropharyngeal cancers associated with high-risk HPV in men who engage in unprotected sexual activity. In women, the infection with this virus has been linked to reproductive issues, as surgeries to remove lesions caused by the virus are necessary. However, a significant biochemical link between infertility and being carriers of high-risk HPV has not been observed in women.
The general population, especially men, is largely unaware of the consequences that can arise from the transmission of this virus. Men, even when they are carriers, do not undergo regular check-ups and unknowingly transmit the virus to all their sexual partners, since the potential consequences are long-term rather than immediate. Fortunately, in 2008, free vaccination began for girls at the age of 12, and as of last year, though in my opinion too late, the vaccine is also being administered to boys of the same age group.
The published study links high-risk HPV carriers with infertility in men. These men showed significantly higher levels of sperm necrosis and a greater proportion of sperm with reactive oxygen species, responsible for the oxidation and fragmentation of sperm DNA, which can block cell divisions and, therefore, embryo development, as well as cause miscarriages during the first trimester. Additionally, a reduction in semen leukocytes and inflammatory cytokines (IL-6 and IL-1β) was observed in this group of men. It is important to note that these adverse effects are not detected in routine semen analyses when a couple seeks assistance from reproductive clinics.
The authors suggest thorough HPV screening in men, including genotype determination, in urology and fertility clinics, which I agree with, as more conclusive evidence could be obtained to corroborate the data from this study, which still has a low sample size to fully understand the importance of this infection in male infertility.
Xavier Bosch - Fertilidad varones y VPH EN
Xavier Bosch
Emeritus researcher at the Catalan Institute of Oncology (ICO), senior researcher at the Bellvitge Biomedical Research Institute (IDIBELL) and lecturer in the Faculty of Health Sciences at the Universitat Oberta de Catalunya (UOC)
Research on HPV initially focused on its etiological relationship with cervical cancer, the most severe and frequent consequence of persistent infections. Now we are broadening the scope with information about the potential medium- to long-term consequences of these infections, including non-tumoral pathology. Research on the natural history of infection in men and fertility is very limited and complex. The data from this study should be taken with caution, and conclusions and clinical implications need to be consolidated and reproduced in other studies.
The study is appropriate in its standardization of diagnostic techniques and methodology. It should be a good contributor to exploring the main hypothesis (infertility in HPV carriers in semen).
Evidence is still accumulating on this topic. Most fertility clinics have already adopted screenings of semen samples for HPV in the evaluation of male-origin infertility. The problem is that we do not have treatments for HPV infection, and therefore, the clinical implications are limited.
[Regarding the study's limitations] I believe it is appropriate to publish it in its current state, which I understand has already been peer-reviewed by specialists in the field.
Rocío Núñez Calonge - Fertilidad varones y VPH EN
Rocío Núñez Calonge
Scientific Director of the UR International Group and Coordinator of the Ethics Group of the Spanish Fertility Society
HPV (human papillomavirus) is the most common sexually transmitted disease, responsible for 95% of cases of the fourth most common type of cancer in women, cervical cancer. This cancer causes approximately 350,000 deaths each year, mainly in low- and middle-income countries.
Public health authorities in 37 countries currently vaccinate girls aged nine to 14 years, before they begin sexual activity. It is also known that HPV increases the risk of genital warts and cancers of the penis, anus, mouth, and throat in infected men, which is one of the reasons why the WHO and the United States Centers for Disease Control and Prevention (CDC) recommend that boys also be routinely vaccinated against it. HPV infection has been found in the semen of approximately 10% of men in the general population and in approximately 16% of men with unexplained infertility, although these data appear to be widely underestimated according to clinical experience. In particular, HPV infection in semen appears to be more related to asthenozoospermia (low sperm motility) and anti-sperm antibodies (ASA) (Garolla et al.).
HPV includes high-risk (HR-HPV) and low-risk (LR-HPV) viruses. The former have a high risk of developing malignant neoplasms, while the latter mainly cause benign warts. Despite growing awareness of the impact of HPV on men's health, the influence of urogenital HR-HPV and LR-HPV infections on male fertility potential remains uncertain.
Rivera and his collaborators have published an interesting study aimed at investigating whether male urogenital infection with HR-HPV or LR-HPV is associated with poor sperm quality, oxidative stress, and inflammation. To do this, they studied the effects of the virus in a representative sample of the male population in Argentina: 205 adult male volunteers who attended a single urology and andrology clinic for an initial evaluation of fertility or urinary tract problems between 2018 and 2021. None had been vaccinated against HPV. The volunteers donated a semen sample, and the presence or absence of HPV and other sexually transmitted infections was determined by PCR.
Of the 205 individuals analyzed, 19% tested positive for HPV. Specifically, 20 men were classified as positive for HR-HPV, while seven were identified as positive for LR-HPV. These HPV-positive individuals were compared with 43 men with no detected infections. Another 12 men were found to be HPV positive, but their genotype could not be determined due to low viral loads.
First, the researchers studied the semen samples following WHO analysis criteria. According to these criteria, they found no evidence of a difference in semen quality between the three groups. However, when Rivero and his colleagues examined the samples with more specific and high-resolution methods, they found that HR-HPV-positive men had significantly lower counts of CD45+ white blood cells (leukocytes) in their semen. They also found evidence that the sperm of HR-HPV-positive men may suffer frequent damage from oxidative stress, as indicated by their elevated production of reactive oxygen species (ROS).
While low levels of ROS are a product of normal sperm function, elevated levels can lead to cell membrane disruption, DNA breaks, and uncontrolled, unprogrammed cell death. In fact, the researchers demonstrated that HR-HPV-positive men had a higher percentage of dead sperm.
"We concluded that men infected with HR-HPV, but not men infected with LR-HPV, show increased sperm death due to oxidative stress and a weakened local immune response in the urogenital tract," said Rivero. "These results suggest that HR-HPV-positive men might have impaired fertility." Rivero and colleagues explained the lower observed count of immune cells in the semen of HR-HPV-positive men due to HPV's known ability to evade an immune response. This would lead to reduced leukocyte movement to the site of HPV infection and their impaired ability to eliminate this infection.
"Our study raises important questions about how HR-HPV affects sperm DNA quality and what implications this has for reproduction and offspring health. It is important to understand the biological mechanisms underlying these effects. And, since sexually transmitted coinfections are quite common, we plan to explore whether having HPV infection along with other STIs influences these outcomes," said Rivero.
Although most published works on the influence of HPV on male fertility show that the infection can affect semen quality, the mechanism by which the virus acts is not known. The importance of Rivero's work lies in differentiating HPV into high-risk or low-risk viruses. In the first case, there is a deterioration in semen quality and, more importantly, a higher likelihood of serious pathologies. This lack of separation between HPV types may be the cause of contradictory results found in other publications. This difference between HPV types is more important than the observation of increased oxidative stress, impaired immune response, and cell death, as these phenomena are a direct consequence of such an infection.
From the perspective of fertility, it is also important to consider not only how the virus may affect sperm, but how sperm may transport it to the female reproductive tract during sexual intercourse, potentially causing female pathologies and infertility. Therefore, while emphasizing the vaccination of not only girls but also boys, the study opens a new avenue of knowledge in which it would be necessary to study infected individuals to determine the type of virus: high or low risk.
Although Rivero's work is promising in terms of understanding the biological mechanisms of human papillomavirus, it has some limitations, such as the low number of cases included in the study. Moreover, the comparison between the group of infected patients and the control group of healthy patients involves assuming that the low semen quality in the former is due to the virus, without knowing what it was like before the infection.
C. Olivera et al.
- Research article
- Peer reviewed
- Observational study
- People



