Injection of CAR-T cells reverses asthma in mice
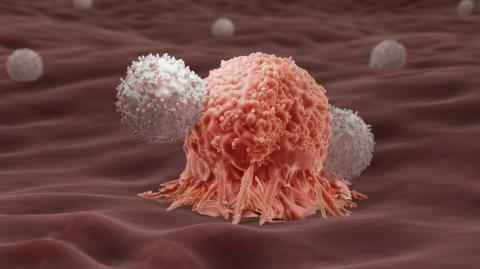
Chinese researchers have designed an asthma treatment based on CAR-T cells. A single injection of these cells, modified to attack the eosinophils themselves - a type of white blood cell that is activated by certain infections and allergies - achieved remission of the signs and symptoms of the disease for at least a year in mice. According to the authors, the technique will need to be tested in human clinical trials, but could be useful for treating both asthma and other types of allergies. The results are published in the journal Nature Immunology.

Soto - CART (EN)
José Gregorio Soto Campos
Director of the Pneumology and Allergy Clinical Management Unit of the Hospital de Jerez
I think this is a high-quality study in basic research. T-lymphocytes are cells of the immune system that are involved in the body's defence against infections and also act against cancer cells. To carry out this treatment, T-lymphocytes are obtained from the patient's blood in a procedure called apheresis: these T-lymphocytes are genetically modified in the laboratory so that they can bind to specific proteins (antigens) expressed on cancer cells and selectively destroy them. These T-lymphocytes, once modified and multiplied in the laboratory to produce millions of lymphocytes that can fight the disease, are then injected back into the patient intravenously. It is therefore a personalised treatment for each patient.
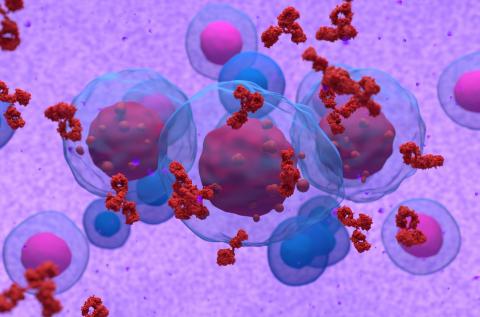
The chimeric antigen receptor (CAR) T-cell therapy programme offers a new cancer immunotherapy that involves genetically modifying T-cells to activate the immune system to recognise and destroy certain types of cancer. CAR T-cell therapy is not the same as stem cell transplantation or chemotherapy. CAR T-cell therapy may be a treatment option for different types of haematological tumours, as well as other cancers and medical conditions that are undergoing clinical trials. Its usefulness in asthma has not been studied, but this study opens up new opportunities.
Depletion of eosinophils using anti-IL-5Rα antibodies alleviates asthma symptoms and reduces the need for medication, such as glucocorticoids. While long-term eosinophil depletion by antibodies is safe, it requires repeated doses and may lose efficacy when patients develop anti-drug antibodies.
Asthma is characterised by eosinophilia driven by interleukin (IL)-5, along with inflammation and airway remodelling caused by IL-4 and IL-13. In the study, they use IL-5 as a targeting domain to engineer long-lived chimeric antigen receptor (CAR) T cells that can eradicate eosinophils. We call these cells functional, immortal CAR IL-5 CAR T cells (5TIF). The 5TIF cells were further modified to secrete an IL-4 mutein that blocks IL-4 and IL-13 signalling, termed 5TIF4 cells. In asthma models, a single infusion of 5TIF4 cells into fully immunocompetent mice, without any conditioning regimen, led to sustained suppression of lung inflammation and relief of asthmatic symptoms. These data show that asthma, a common chronic disease, can achieve long-term remission with a single dose of long-lived CAR T cells.
In terms of limitations, although 5TIF4 cells represent engineered immune cells capable of paving the way for and replacing biologic therapy that requires repeated, lifelong administration, such therapies have not been tested in chronic respiratory diseases and we do not know about their potential adverse effects in humans.
Jin et al.
- Research article
- Peer reviewed
- Experimental study
- Animals