The meningococcal B vaccine may provide partial protection against gonorrhoea
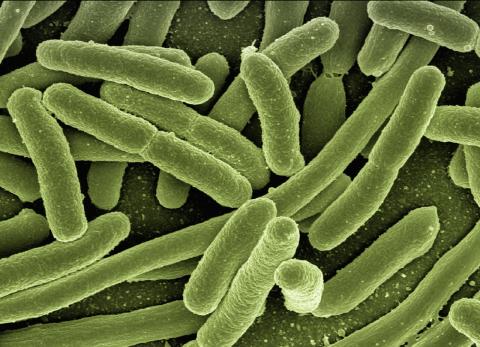
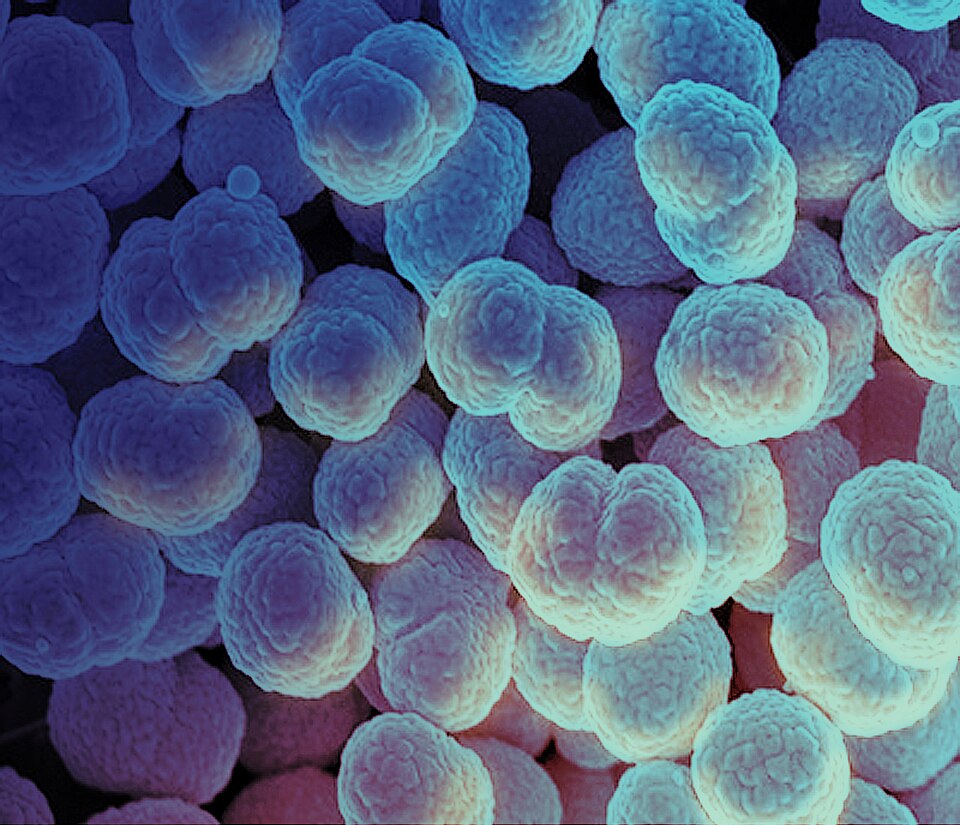
Gonorrhoea is the second most common sexually transmitted disease in the world, with 80 million cases each year. There is no effective vaccine, and the bacteria responsible are becoming resistant to common antibiotics. Some studies have suggested that the meningococcal B vaccine, a unrelated bacterium, may offer partial protection against gonorrhoea. Now, an Italian team has identified 17 antibodies that could explain this cross-immunity, which, according to the authors, could be used to develop treatments and vaccines. The results are published in the journal Science Translational Medicine.
Santiago Moreno Guillén - gonorrea EN
Santiago Moreno Guillén
Head of the Infectious Diseases Service at Ramón y Cajal Hospital (Madrid) and professor in the Department of Medicine at the University of Alcalá de Henares.
Attempts to prevent gonorrhoea through cross-immunity conferred by the meningococcal vaccine have been explored previously, and clinical trials have even been conducted. In this study, the authors conducted an in vitro study and animal experiments. Basically, their main finding is the identification of antibodies developed after vaccination against meningococcus B (in three healthy volunteers) that would kill gonococcus in vitro. I am not in a position to judge whether the work is technically sound, although I imagine it is, given that it has been published in this journal.
What I can judge is the scope of the results: they are extremely preliminary data, with possibly little scope for further development. I say this based on recent data. A clinical trial for the prevention of bacterial sexually transmitted infections (gonorrhoea, syphilis and chlamydia) was recently published. It evaluated the effect of doxycycline in preventing these three infections and the meningococcal B vaccine (the same as in the study) in adding protection against gonorrhoea. The conclusions were that doxycycline works against syphilis and chlamydia, and that the vaccine does not add any protection against gonorrhoea.
The authors comment that the antibodies generated that have been shown to be effective could be transferred passively for prevention, as has been done with antibody transfers in the case of COVID-19, but this does not make much sense; it is preferable to administer the vaccine.
Troisi et al.
- Research article
- Peer reviewed
- People