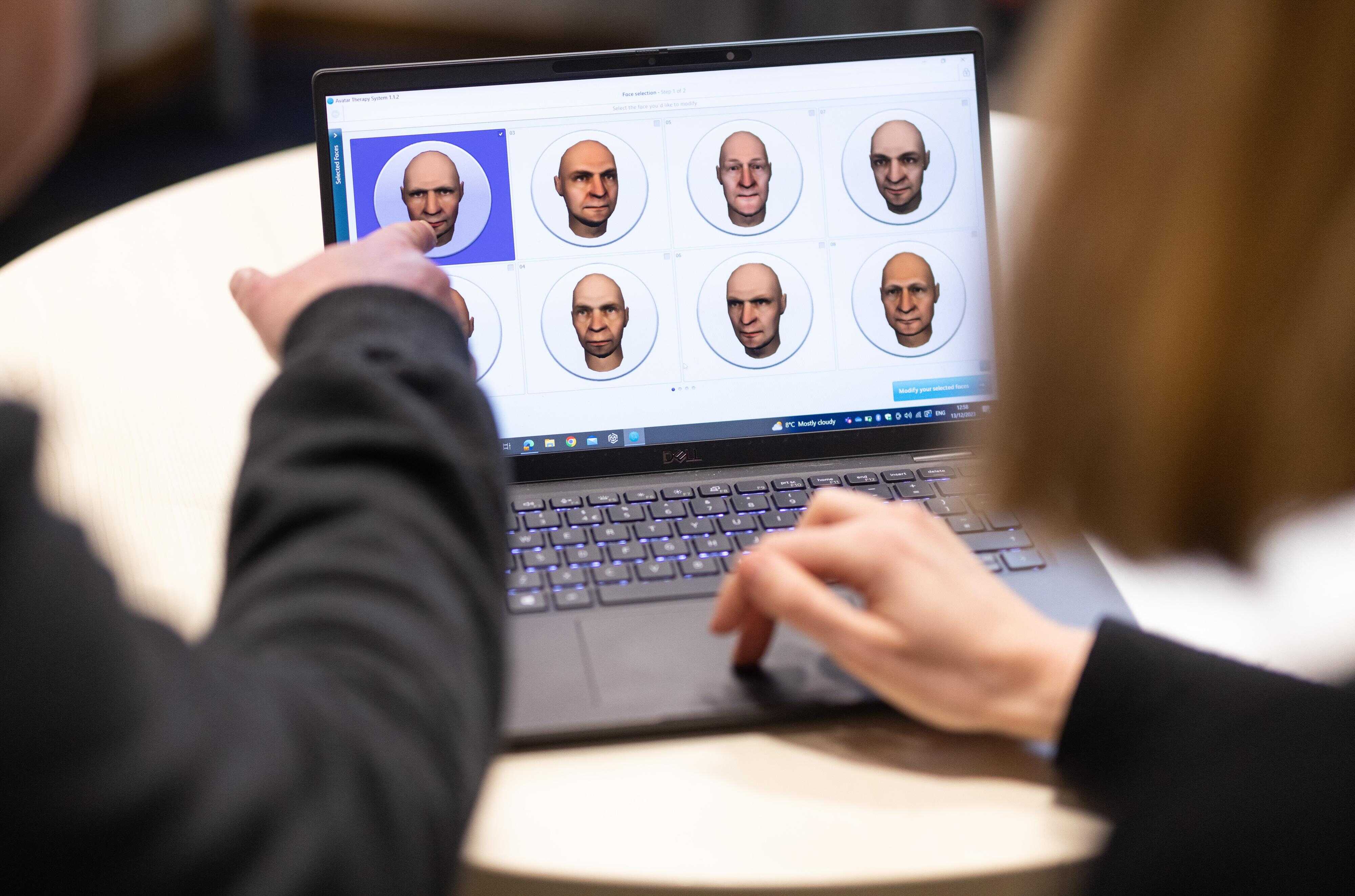
Clinical trial tests digital avatar to treat voices in people with psychosis
A team of researchers from the United Kingdom has conducted a phase 2/3 clinical trial in people with a psychotic disorder to study the efficacy of interaction with a digital avatar in alleviating the discomfort generated by hearing voices. After analyzing it in 345 people, they conclude that it can reduce the frequency of occurrence at 16 and 28 weeks. The discomfort provoked is reduced at 16 weeks, but not at 28 weeks. The team publishes the results in the journal Nature Medicine.
Celso Arango - avatar psicosis EN
Celso Arango
Head of the Department of Child and Adolescent Psychiatry and Director of the Institute of Psychiatry and Mental Health of the Hospital General Universitario Gregorio Marañón
This phase 2/3 clinical trial compares treatment as usual versus treatment as usual but with the addition of two forms of avatar therapy in people with psychotic disorders who have auditory hallucinations that produce distress. One of the two added treatments was a simpler, six-session, non-personalised treatment based on exposure, assertiveness and self-stigma. The second, with twelve sessions, was personalised for each participant, integrating each patient's personal history into the intervention through the avatar.
Both avatar interventions were more effective than treatment as usual in reducing distress caused by auditory hallucinations (primary endpoint) at 16 weeks of treatment. Neither avatar intervention was superior to treatment as usual at 28 weeks, the severity of auditory hallucinations was also reduced at 16 weeks with both interventions, and the frequency of auditory hallucinations was reduced at 28 weeks only with the more personalised avatar intervention.
The study is very well conducted, with a sufficient sample size to assess the primary endpoint, and adds evidence for the use of digital innovation in the treatment portfolio for people with mental disorders.
However, several questions remain unresolved, such as identifying which patients can benefit from this treatment, especially since only 58% of those who were assigned the most personalised treatment completed the study. It is also necessary to know by what mechanism the reduction in discomfort is produced. It is hypothesised, but unanswered, that it may be by reducing anxiety and feelings of threat, greater empowerment or acceptance of voices. The two interventions have not been compared with psychotherapies that have been shown to be effective in these cases, such as cognitive-behavioural therapy (CBT) and cognitive-behavioural therapy (CBT). Given the lack of people who can carry out these psychotherapies in the public system, cost-effectiveness studies are needed. If these digital interventions are shown to be cost-effective, they could become an alternative for a group of people with psychotic disorders.
Alberto Ortiz - avatar psicosis EN
Alberto Ortiz Lobo
Doctor of Medicine and Psychiatrist at the Carlos III Day Hospital - La Paz University Hospital (Madrid)
The study suggests the benefit of ‘embodying’ the voices presented by people with psychosis in an avatar in order to reduce their distress. A limitation of the research is that it compares adding this intervention to standard treatment with not adding it, but not with any other type of intervention or technique. The results are unpromising because they find a significant difference in improvement at 16 weeks that is lost when the results are measured at the end of the study, at 28 weeks.
In any case, we should consider who will benefit from delimiting and externalising this specific experience and what impact ‘personalising’ voices through an avatar may have on them in the medium and long term. This is crucial because hearing voices is not an isolated or unique problem for people diagnosed with psychosis, but a further expression of their psychological suffering, which requires a holistic and contextualised view and understanding of their biography and environment.
Valdecasas - Voces (EN)
José García-Valdecasas
Psychiatrist, Vice-Secretary of the Board of the Spanish Association of Neuropsychiatry
The study follows a fairly current line of research that seeks to implement digital solutions for the treatment of different psychiatric pathologies, in general, with poor results.
The data speak of a certain efficacy at week 16, which is not maintained at week 28. It is true that current treatments with psychotropic drugs or psychotherapy are sometimes not helpful enough, but there are approaches, for example, in mutual support groups of voice listeners, which seem more promising, in my opinion.
In addition, some of the authors have conflicts of interest to consider, with companies dedicated to these digital tools, which I believe may affect their judgment.
It does not seem to me that these findings will have clinical relevance.
Conflict of interest: “I have had no conflicts of interest with pharmaceutical or medical device companies for about 15 years".
Garety et al.
- Research article
- Peer reviewed
- Clinical trial
- People



