Reaction: Malaria vaccine shows protection in clinical trial
An experimental malaria vaccine has shown protection for at least six months, according to a clinical trial in 112 adults in Burkina Faso. The results are published today in the journal Science Translational Medicine.
Consuelo Giménez - vacuna malaria EN
Consuelo Giménez Pardo
Professor of Parasitology at the University of Alcalá (UAH) and director of the Master's Degree in Humanitarian Health Action (UAH-Doctors of the World)
In very general terms, the study seems methodologically sound, although the number of patients is not specified in the material and methods, which is then shown in the tables to be very low. The geographic location of the study, only in Burkina Faso, makes it risky to conclude in a blunt manner that "with three doses of the vaccine, it can be used for seasonal protection for 4-6 months in children aged 2-12 years in sub-Saharan Africa".
The history of malaria vaccine trials over the years makes us too cautious to state absolute truths; I understand that a much larger study both in number and geographic location is needed to make this assertion.
In fact, it is worth reviewing the attempts to generate an efficient and effective malaria vaccine, which have been numerous throughout history, but I will focus on two of them because of their relevance: Manuel Elkin Patarroyo's SPf66 vaccine and Glaxo-SmithKline's RTS,S, validated by Pedro Alonso.
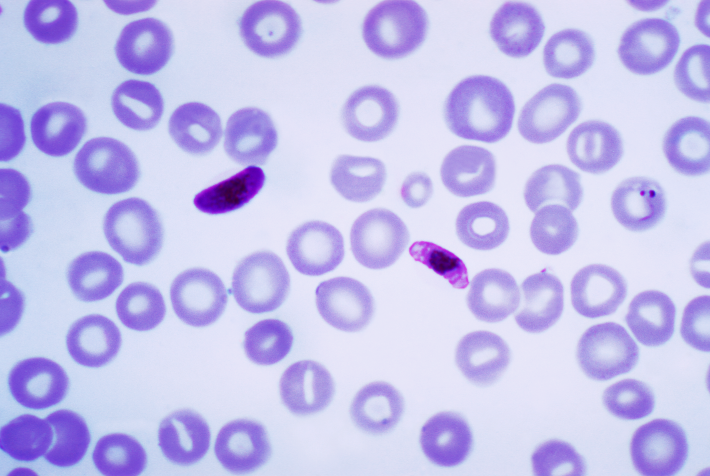
In the 1990s, hope opened up with the development of SPf66, a synthetic or recombinant subunit vaccine, an "antigenic cocktail", with the proteins necessary for parasite survival (those with low mutation rates and conserved epitopes), capable of reducing severe and complicated malaria and malaria-related mortality. Referred to as the "Colombian vaccine", it showed protective efficacy ranging from 38.8% to 60.2% against Plasmodium falciparum malaria. Finally, after further clinical evaluations, the World Health Organisation (WHO) classified it as inactivated. With the new millennium, a pre-erythrocytic vaccine candidate generated by Glaxo-Smithkline in 1987 and called RTS, S/AS02A, based on Plasmodium falciparum circumsporozoite surface antigen was shown to be effective in phase 2 in Mozambican children aged 1-4 years against clinical malaria risk of 35.3% and against severe malaria of 48.6% marketed as Mosquirix™. After decades of clinical development, it has been the first malaria vaccine to be tested in phase 3 clinical trials and now in implementation studies.
In 2019, three countries, Ghana, Kenya and Malawi, have introduced RTS,S in a WHO-coordinated programme so that, by October 2020, nearly half a million children have received the vaccine in areas where they are at high risk of malaria illness and death, achieving a 40% reduction, as WHO, Gavi26, and other groups weigh the risk-benefit, cost-effectiveness and practical issues of vaccine implementation capacity in resource-limited settings.
Vector control prevention measures that we know work, such as insecticide-treated bed nets and indoor spraying, sulphadoxine-pyrimethamine treatment in pregnant women, and seasonal chemoprevention in children, need to be employed.
One of the problems that can increase the number of deaths and that requires special attention is the difficult access to antimalarial treatments, as well as the interruption of treatments already started. As mentioned above, this is a titanic struggle with the ultimate goal of malaria eradication because it will have an impact on improving the health of populations in relation to poverty and because of the need for social justice for those living in endemic regions.
Sodiomon B. Sirima et al.
- Research article
- Peer reviewed
- Clinical trial
- People



