Reactions: data from Alzheimer's clinical trial with lecanemab antibody published
A few weeks ago, a press release from the Biogen and Eisai companies reported significant results from their lecanemab antibody for the treatment of early-stage Alzheimer's. The data from the phase 3 trial are now published in the New England Journal of Medicine, coinciding with the CTAD conference on Alzheimer's disease clinical trials in San Francisco. Data from the phase 3 clinical trial are now published in the New England Journal of Medicine, coinciding with the 15th CTAD Alzheimer's disease clinical trials conference in San Francisco.

Fortea - Lecanemab (EN)
Juan Fortea
Director of the Memory Unit of the Neurology Service of the Hospital de la Santa Creu i Sant Pau and director of the Alzheimer's Unit at the Fundació Catalana Sindrome de Down
The study is very robust. The essential data on efficacy, slowing disease progression by 27%, we already knew, but they gave secondary clinical and biomarker results and they are all very consistent and in the same direction. The safety data, despite some alarmist reports, also seem reasonable. The side effects are less than with aducanumab [an FDA-approved anti-amyloid antibody in the US]. Overall, I think they have cleared up a lot of doubts.
The implications will be very important for the field, as it will probably be the first disease course-modifying treatment. The currently approved drugs are symptomatic, I don't think it's appropriate to compare them. At this conference, the idea that clinical response depends on whether you actually remove amyloid (Roche's ganterenumab removed much less than expected and it is thought that this may be the reason [for the failure of their clinical trial]; in a post-hoc analysis they found that those who had the most amyloid reduction got less worse) has gained a lot of traction. It will be very important to see the dose-response analyses on ganterenumab and lecanemab; and of course, donanemab [another anti-amyloid antibody developed by the Eli Lilly company] coming out in the spring.
In terms of limitations, I don't see any relevant scientific limitations, the data are very solid. It is true that the efficacy is modest (27%) and that the consequences are dizzying. But the vademecum would be significantly slimmed down if the bar were set here, and I don't think the detractors are proposing to discriminate against Alzheimer's disease over other diseases.
The only limitation, more political than scientific, is that the EMA (not the FDA) always asks for 2 trials. This is a giant one (1800 patients, compared to Roche's two trials of 900 each). I understand that Eisai/Biogen pre-agreed the trial conditions with the FDA and EMA, but we will see what happens in Europe.
I have been a consultant or been on advisory boards for several companies with anti-amyloid antibodies, including Roche, AC Immune or Novartis and I have given talks for several other companies, including Biogen. However, my main "COI" is scientific, I did my thesis on ADAD (Autosomal Dominant Alzheimer's Disease) and I am the director of an Alzheimer Down unit. These populations are the strongest evidence in favour of the amyloid hypothesis.
Marc Suárez - alzheimer NEJM EN
Marc Suárez-Calvet
Researcher at the Barcelonabeta Brain Research Center and the Neurology Service of the Hospital del Mar (Barcelona)
The Clarity study is a phase III, multicentre, randomised, double-blind, phase III clinical trial testing the anti-amyloid monoclonal antibody lecanemab compared to placebo in patients with early-stage Alzheimer's disease.
The clinical trial demonstrates its main objective: there is less cognitive and functional impairment in the treatment arm compared to the placebo arm. Using the CDR-SB scale (ranging from 0 to 18; a higher value means greater cognitive and functional impairment), patients in the placebo arm have an average increase of 1.66 points over the 18-month follow-up, while those treated with lecanemab only have an increase of 1.21 points. The study also shows that lecanemab treatment significantly reduces amyloid accumulation in the brain. Finally, lecanemab treatment is also better than placebo on all secondary endpoints studied, including other cognitive scales and biological biomarkers. In conclusion, this is a well-designed, rigorous study that points to a beneficial effect of lecanemab in the early stages of Alzheimer's disease.
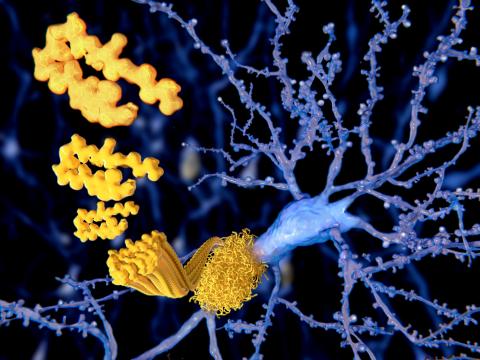
Lecanemab, unlike other anti-amyloid antibodies, has a special affinity for soluble amyloid protofibrils, which probably have a toxic effect in the brain. This feature is possibly one of the reasons for its good results.
While it is true that the study shows less cognitive decline in patients treated with lecanemab, the clinical relevance will have to be determined. A difference of 0.45 on the CDR-SB scale, which ranges from 0 to 18, may seem minor. However, small changes in cognition can have a big impact not only on patients' autonomy, but also on their caregivers. On the other hand, we should bear in mind that the trial investigates the effect of the drug after 18 months of administration. Longer studies will have to be carried out to determine the long-term effect.
The aim of this study is not only to determine the efficacy of the drug, but also its safety. There is no difference in the number of deaths or total number of adverse events between the lecanemab arm and the placebo arm. However, there is a higher proportion of amyloid-related imaging abnormalities (ARIA). Although these abnormalities are not serious in most cases, they need to be studied in detail. Also, it has recently been reported that two people included in the trial died. Whether these deaths are attributable to the drug or to other reasons needs to be studied. As Alzheimer's is a heterogeneous disease, it will be important to determine which patients can potentially benefit most from this treatment and which of them have a higher risk of side effects. The same study shows that it is patients with allele 4 of the APOE gene who are most at risk of adverse effects in the form of ARIA. Treatment and doses administered to these patients will probably need to be individualised.
Raquel Sánchez - alzhéimer NEJM EN
Raquel Sánchez-Valle
Head of the Neurology Department at Hospital Clínic de Barcelona and secretary of the Spanish Society of Neurology's Study Group on Behaviour and Dementia
Following the press release from Eisai Pharmaceuticals on 28 September 2022 regarding the results of the phase 3 study, Clarity, with lecanemab in patients with early Alzheimer's disease (mild cognitive impairment and mild dementia due to Alzheimer's disease), we are awaiting the presentation of the scientific results that has taken place simultaneously at an international congress (CTAD 2022) and with the publication of the peer-reviewed results in the New England Journal of Medicine.
The first conclusion from reading the published article is that the announced results hold after peer review. The analysis of the primary efficacy endpoint (sum of Clinical Dementia Rating-CDR-SOB boxes) shows a significant benefit of lecanemab treatment at 18 months of treatment. The difference between the active group and placebo on the primary endpoint with the specified statistical treatment was -0.45 points on CDR-SOB (decline of 1.21 points in the lecanemab arm and 1.66 in the placebo arm), which is 27% less worsening in the active arm. This result is statistically positive (the study was designed to identify a difference of 25% or more). All four pre-specified endpoints also showed a positive effect for lecanemab. This indicates that the trial shows an overall positive outcome, with results on the different pre-specified endpoints congruent with each other, in line with the results of previous studies with this drug.
Regarding the clinical effect, the publication concludes that it is modest. The study was designed to identify a 25% difference at 18 months on the CDR-SOB scale after consultation with regulatory authorities and experts. My reading is that the proposed target, based on the data shown in the publication, has been met. There is currently no consensus on what magnitude of change on the scale chosen by previous consensus (CDR-SOB) is to be considered clinically relevant. Moreover, previous literature indicates that patients, clinicians and payers (who include cost as well as benefit in the assessment) may have a different opinion in this regard. I do not believe that the effect can be compared with symptomatic drugs available for mild-moderate stages of dementia, as the target population and study design are different, and changes on a given scale are not linear over the course of Alzheimer's disease. Longer-term data will be needed to know whether this clinical effect is maintained, increased or transient to understand its potential clinical impact.
Tracer uptake marking amyloid in plaques, which was included as a secondary endpoint, was significantly reduced in treated patients, and although no data is provided on the percentage of patients who tested negative in this test, it is indicated that the mean level of tracer uptake was below the amyloid-positive threshold at 18 months, indicating that the clinical effect could be associated with a dramatic reduction in the amyloid burden in treated patients.
21.5% of those treated with lecanemab had one of the MRI abnormalities that have been associated with amyloid (ARIA), compared to 9.5% in the placebo arm. These alterations were more frequent in carriers of the ε4 genotype of the APOE gene, indicating that, although these alterations can appear spontaneously in patients with Alzheimer's disease, this anti-amyloid treatment increases their frequency, especially in the most genetically susceptible patients. While most of these alterations were not accompanied by symptoms, 3.5% of patients receiving lecanemab had symptoms related to these MRI alterations. Of those receiving lecanemab, 5 subjects (0.6%) experienced a brain haemorrhage and 1 (0.1%) of those receiving placebo. More infusion-related reactions were also reported in the active arm (26.4% vs. 7.4%). There were 6 deaths in the treatment arm and 7 in the placebo arm, although none of the deaths were attributed to the drug. These effects are in my opinion relevant and require close monitoring of the drug, especially in the first months, and knowledge on the part of patients receiving the drug, but I believe that they are per se a reason, at this time, to avoid its use.
Recently, different press sources have reported a case of a patient who died during the open-label phase of the study. This patient had a brain haemorrhage immediately after being treated with rtPA, a drug administered to try to break up a thrombus after a stroke. It is well known that a percentage of patients treated with rtPA have a brain haemorrhage as a complication, and that this percentage is higher in patients with amyloid in their cerebral vessels. From the data that have been made public, I do not believe that the haemorrhage that led to this patient's death can be attributed to the direct effect of lecanemab, but rather to rtPA. Another thing is that we will have to analyse the case and assess whether it is safe to use rtPA in patients receiving lecanemab or whether it should be avoided, as we know it should be avoided in other clinical situations and with other drugs.
The FDA announced that on 6 January 2023 it will communicate its decision on the approval of lecanemab under the accelerated approval pathway. Patient and professional associations are likely to comment on the outcome of lecanemab in the coming weeks. Regulatory authorities are likely to not only analyse the study results, but also consider stakeholders' views on efficacy and tolerability.
Raquel Sánchez-Valle has participated in the Clarity study as principal investigator of the study at the Hospital Clínic de Barcelona. The centre has received funding for the study, but Raquel Sánchez-Valle has not received personal compensation for her participation.
Van Dyck et al.
- Research article
- Peer reviewed
- Clinical trial
- People