Reaction: CRISPR used to protect mice from heart disease
Ischaemia-reperfusion injury is one of the causes of damage caused by diseases such as myocardial infarction. A study published in the journal Science has used base editors, a gene-editing tool derived from CRISPR, to modify a key protein in the hearts of mice. According to the authors, the intervention allowed them to recover their function after a heart attack and could potentially be used in a wide range of patients, as it does not depend on the presence of a specific mutation.
Lluís Montoliu - CRISPR cardio EN
Lluís Montoliu
Research professor at the National Biotechnology Centre (CNB-CSIC) and at the CIBERER-ISCIII
On the last day of 2015, three laboratories released their independent results of using first-generation CRISPR gene-editing tools to treat a mouse model of Duchenne muscular dystrophy by removing a fragment of the dystrophin gene, which carries the mutation that causes the disease. One of these laboratories was that of Eric N. Olson at the University of Texas Southwestern Medical Center in Dallas, one of the first to demonstrate that CRISPRs could be administered directly into animals, encapsulated in viral vectors, to treat congenital diseases.
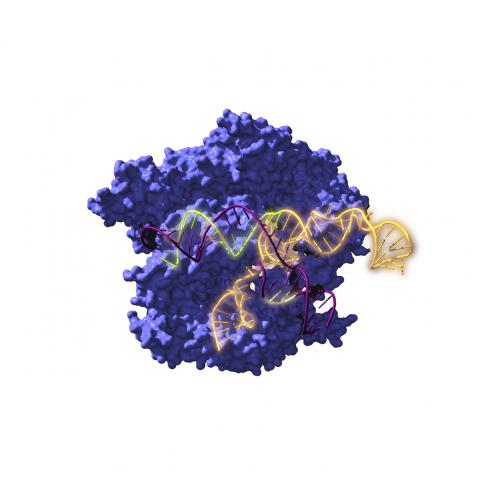
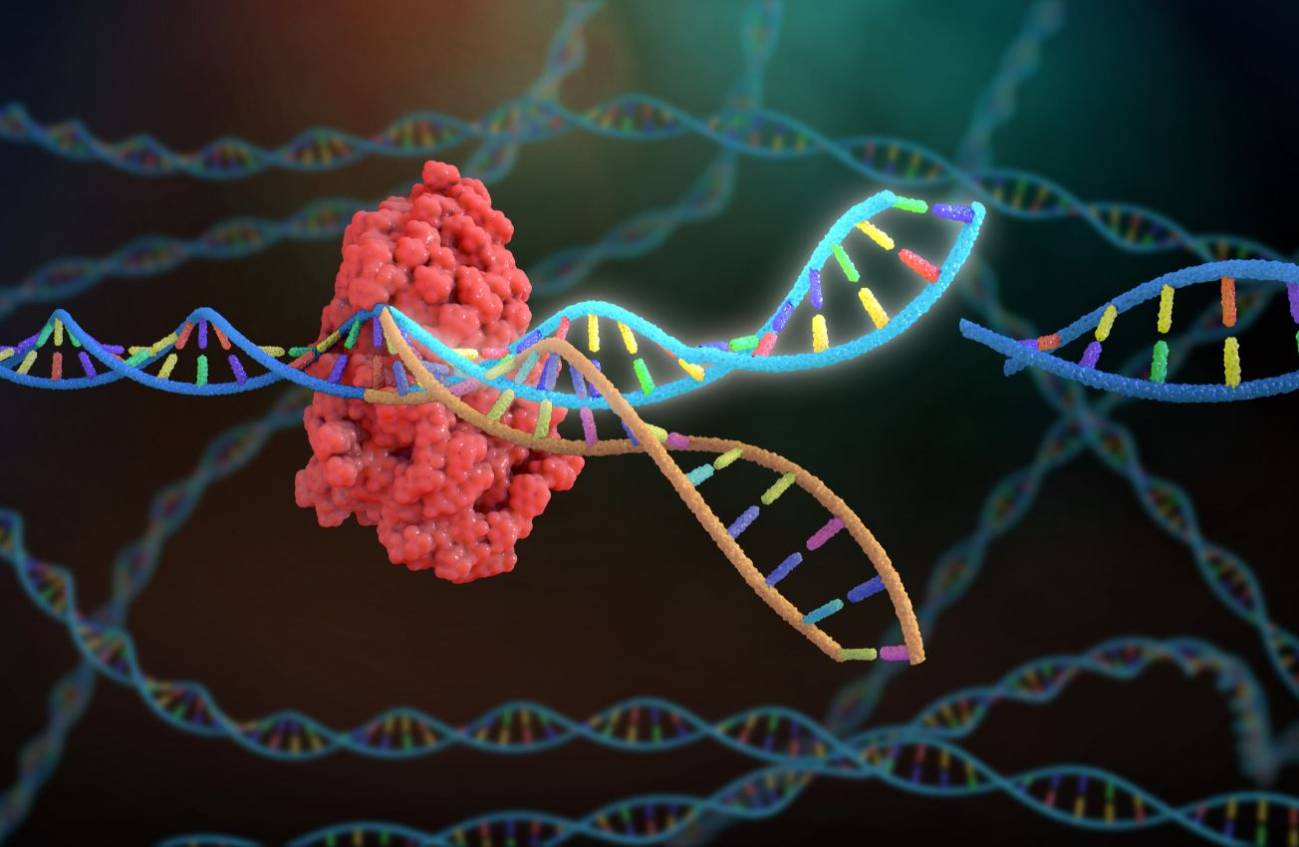
Seven years later, the same lab has once again surprised us with a new use of the most advanced CRISPR tools, the base editors, capable of chemically changing letters in the genome (for example, an A for a G) without cutting the DNA and, therefore, with greater safety. In this work by Lebek and colleagues, Olson's lab decided to use a base editor to change two amino acids (two methionines) in a protein kinase called CaMKIIdelta, which when oxidised and reactivated causes serious heart disease. The amino acid methionine is encoded by the ATG triplet, which the authors change to GTG, now encoding the amino acid valine, which can no longer be oxidised or serve to reactivate the protein.
The authors cleverly evaluate their strategy first in cultured cells, in human cardiomyocytes derived from inducible pluripotent stem cells (iPS), and select the best CRISPR reagents for base editing. They then injected viral vectors carrying these reagents into the hearts of mice that had suffered an experimental heart attack and observed the recovery of cardiac function. This early preclinical evidence suggests that something similar could happen if the same CRISPR reagents were injected into the infarcted area of a human heart, but this is still some time away from being investigated. Further preclinical animal studies are needed to assess the safety and efficacy of the procedure in the short, medium and long term.
The use of CRISPR tools is not innocuous. Neither is the use of base editors. Beyond the bases that are intended to be modified, the system can end up changing other nearby bases in the genome's target sequence or in other genes that present similar sequences, compatible with the RNA guide that serves to direct the base editors to the selected gene. Some of these situations can be predicted with computers. Others cannot and must be investigated experimentally. The authors find unexpected modifications of both types, in other bases close to the ones they want to modify in the same gene and in other similar genes. Fortunately, they reason that none of these unwanted modifications seem to affect the development of their experiments, but this is more a product of chance than of the researchers' will. More optimised base editors that fundamentally alter the intended sequences, without significantly affecting other parts of the genome, should therefore be further investigated.
This new study confirms the trend observed over the past two years of the rapid evolution of CRISPR tools, with base editors (originally described by David Liu of the BROAD Institute in 2016) predominating in therapeutic approaches, due to their greater precision and safety. However, as this latest study shows, they are not yet complete and require further research.
Lebek et al.
- Research article
- Peer reviewed
- Animals