Reactions: gel stops brain tumors in mice
A drug in gel form cured 100 percent of mice with a very aggressive brain tumor. The authors hope that this is a first step towards helping human patients with glioblastoma, one of the most dangerous brain tumors in humans. The article is published today in PNAS.

Jordi Bruna - reacción gel tumor EN
Jordi Bruna Escuer
Coordinator of the Neuro-oncology Unit of the Bellvitge Biomedical Research Institute (IDIBELL) and researcher of the Neuroplasticity and Regeneration Group of the Autonomous University of Barcelona
The animal model on which the study is based is not at all representative of what a human glioblastoma is. They have worked with a murine cell line that was chemically induced with a series of alterations that morphologically mimic glioblastoma, but which at the molecular level have nothing to do with human glioblastoma. It is often used to study the effects of host immunity. But to claim that the immune reaction of the mouse to this experimental glioma is the same as that of the patient is a considerable leap of faith. There is still a long way to go before the therapy they propose can be tested in patients to assess first safety and then some kind of efficacy.
gel glioblastoma - Pilar Sánchez Gómez
Pilar Sánchez Gómez
Senior Researcher at the Carlos III Health Institute, Head of the Neuro-oncology Unit at the Chronic Diseases Research Unit (UFIEC-ISCIII)
Researchers at Johns Hopkins University, in collaboration with other centres, have found a form of therapy that is capable of eradicating aggressive gliomas in mouse models. These aggressive gliomas, also called glioblastomas, have a very poor prognosis. Patients with such tumours undergo surgery in order to remove as much of the tumour as possible. They are then given several cycles of radiotherapy, combined with chemotherapy with an agent called temozolomide. Despite this aggressive treatment, the tumour always grows back and patient survival is very low (around 5% survival 5 years after diagnosis).
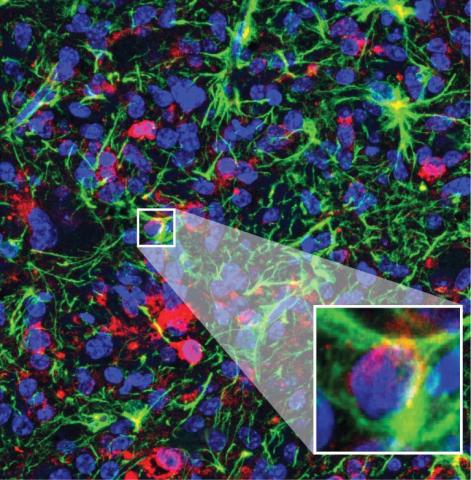
In this study, researchers have designed a strategy to deliver the anti-tumour drug directly into the surgical cavity, so that it reaches the brain more efficiently. To do this, they use a hydrogel containing a drug aimed at slowing the growth of tumour cells, together with a protein designed to encourage the patient's own immune cells to become active and capable of attacking the tumour. With the latter, they aim to make the therapy more effective and, above all, longer-lasting. This strategy is being tested in a mouse model of glioblastoma, the GL261 mouse model, which undergoes 'surgery' and then the hydrogel is deposited with the drug. Although other researchers have published different molecules capable of slowing the growth of these tumours, it is true that the result shown by the researchers in this article is spectacular, as they are capable of completely eradicating the tumour cells. They are therefore able to cure the animals, which is difficult because it is a very aggressive cell line.
One of the handicaps in the treatment of patients with brain tumours, and specifically glioblastomas, is the difficulty for the drug to reach the brain. Several years ago there were already some clinical trials using Gliadel, which consisted of drug-releasing tablets that were deposited in the surgical cavity. In fact, Johns Hopkins University, and in particular some of the researchers in this study, were involved in those trials. Although Gliadel was not shown to be effective in patients with glioblastomas, the great advances in understanding the biology of these tumours, along with improvements in the design of drug-eluting gels, allow optimism for future clinical trials.
Two limitations of the study stand out: on the one hand, the researchers are unable to discern how much of the anti-tumour effect is due to the presence of the anti-tumour agent and how much is due to the activation of the immune response. On the other hand, researchers use a single glioblastoma model which, although widely used in the field of neuro-oncology, has been criticised for not faithfully representing the biology of these tumours, particularly with regard to their interaction with immune cells. This is why trials with other models, either in mice or in models closer to the clinic, have yet to be performed before clinical trials in patients can be designed.
Wang et al.
- Research article
- Peer reviewed
- Experimental study
- Animals