EMA recommends not to approve lecanemab against Alzheimer's disease
The European Medicines Agency (EMA) has recommended not granting marketing authorization for Leqembi™ (lecanemab) for the treatment of Alzheimer's disease. The EMA's Committee for Medicinal Products for Human Use (CHMP) considers that its effect in delaying cognitive decline does not outweigh the risk of serious side effects associated with the drug, in particular swelling and possible bleeding in patients' brains. Leqembi™ was approved in 2023 in the United States.

Lecanemab EMA - John Hardy
John Hardy
Professor of Neuroscience and Group Leader at the UK Dementia Research Institute, UCL.
I have to say I am disappointed in the decision to not grant a license to Lecanemab for the treatment of Alzheimer’s disease. The EMA (in contrast to the FDA) has taken the view that the risk of ARIA outweighs the clinical benefit. The imaging abnormality seen in treated patients is usually either without symptoms or with only minor, headaches as symptoms, but is occasionally associated with brain haemorrhages. The question of whether the undoubted statistical benefit of treatment is worth the risk of serious, though rare side effects is always difficult with any treatment and on this occasion the EMA in Europe and the FDA in the US have reached different conclusions when presented with similar data. I am sure we will now see rich people with early Alzheimer’s disease flying to the US or other jurisdictions for treatment. My guess would be that this decision will be revisited as US clinicians and others gather and report real world experience with both lecanemab and the (very similar) dononemab treatments.
Lecanemab EMA - Tara Spires-Jones
Tara Spires-Jones
Director of the Centre for Discovery Brain Sciences at the University of Edinburgh, Group Leader in the UK Dementia Research Institute, and Past President of the British Neuroscience Association
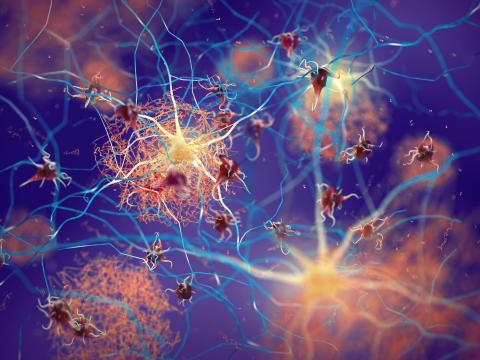
The Phase III clinical trial of lecanemab showed that it does what it’s supposed to; it reduces toxic amyloid in the brain and slows cognitive decline. Scientifically, this was an important step forwards. However, the size of the effect was modest, and coupled with that there were significant side effects, including swelling and brain bleeds leading to death in a few people.
“The EMA’s decision will come as a disappointment to many, but there are reasons to remain hopeful. Lecanemab has shown that it is possible to slow down disease progression, and research does work. Now we need to ramp up our efforts to discover new and safer treatments. Scientists around the world are tackling this from different angles – from stopping toxic “tau” proteins moving through the brain, to protecting synapses, which allow neurons to communicate. Each discovery brings us closer to new and better treatments.
I have no conflicts with this story. Full declaration of financial interests is: Scientific Advisory Boards: Scottish Brain Sciences, Cognition Therapeutics, Race Against Dementia; Charity Trustee: Guarantors of Brain, British Neuroscience Association; Consulting/Honoraria for talks: Jay Therapeutics, Sanofi, AbbVie; Funding lab research: UK Medical Research Council CoEN grant, UK Dementia Research Institute, Alzheimer’s Society.
Lecanemab EMA - Ivan Koycheb
Ivan Koychev
Doctor, Senior Clinical Researcher, Dementias Platform UK, Department of Psychiatry, University of Oxford, Warneford Hospital, Oxford
EMA's decision on lecanamab reflects the complex considerations that had to be taken into account. On the one hand, this is a novel therapeutic option that appears to affect the causes of a devastating condition for which we only currently have symptomatic treatment. An approval would have been a positive sign for further innovation in dementia drug development and create impetus for redesigning the dementia care pathways across the EU and elsewhere. On the other hand, the cognitive benefits for with syndromal stage of Alzheimer's disease are at best modest and occur in the context of significant side effects. In addition, the investment required to deploy this novel treatment for dementia is substantial: an economic analysis showed that the cost of the drug alone equals half of the current medication budget of the EU (assuming it was given to everyone who is eligible).
In my view, the decision creates pressure on EMA to create clear guidance on what clinically meaningful benefit in syndromal Alzheimer's disease is. This will help to maintain the momentum created by the amyloid clearance therapies break-through and offer hope for those living with or at-risk for dementia.
Ivan Koychev has received a grant and speaker fees from Novo Nordisk. He is a paid medical advisor for digital healthcare (Five Lives SAS, Cognes, Cognetivity, Lola Speaks) and biotechnology (CFDX Ltd) companies in the dementia space.
Lecanemab EMA - Mercè Boada Rovira
Mercè Boada Rovira
Neurologist and medical director of Ace Alzheimer Center Barcelona.
Today the EMA has taken the decision not to register Leqembi™ in the EU. This decision brings with it two major concerns, both for the clinical, medical and care community, as well as for the research community. Patients in Europe will be discriminated against, they will not have the same options and opportunities as patients in other countries. And in terms of research and investment in research, Europe will also be in second place.
We will pass the desert again. We will be in the middle of a drought again. And this will affect the quality of patients and their families, the research capacity of Spanish researchers and clinicians and in itself will impoverish our entire healthcare system by not having the opportunity to collect data from the real world (real world evidence) to understand, to improve and to change the frequency-doses of new products that may appear and to invest. To invest especially in the research of treatments much more effective than this one, undoubtedly, for the benefit of our citizens.
This is the position of the Ace Foundation, the clinical department and the research department, and we regret this decision of the EMA.
Lecanemab EMA - Eloy Rodríguez
Eloy Rodríguez Rodríguez
Head of the Neurology Department at the Marqués de Valdecilla-IDIVAL University Hospital and Associate Professor of Medicine in the Department of Medicine and Psychiatry at the University of Cantabria
I consider the decision taken by the EMA to be very negative. Basically two aspects are alluded to: the debatable clinical relevance of the effects and the side effects. Lecanemab has provided solid evidence of its biological effect that corresponds to moderate clinical efficacy in slowing down the progression of the disease in very early symptomatic phases. The clinical impact may seem small, but this is very relative: the results we have are only at 18 months and in patients with such a mild clinical situation a change of 0.5 points on a scale (CDR-SOB) on which the average score is 3.2 at the time of starting treatment (the scale goes from 0 to 18, the higher the score, the worse the clinical condition) means a slowing of progression measured on this scale of 30%.
Who are we to judge whether 6 months more in a clinical situation of mild cognitive impairment (patients who are independent) is too little or too much? We agree that we would all like it to be more, but it is not a negligible change.
But the reason for the rejection is not so much the small clinical efficacy as the potential side effects. In a small percentage of patients (0.8% of serious adverse effects in the CLARITY trial) they are serious (even in a small number of patients they can be fatal). According to the EMA this is not assumable, and this is where the most controversial part lies. Most of these effects appear in ApoE e4 homozygous carriers (15% of patients) or in anticoagulated patients. The first two aspects can be known before starting treatment, they can be discussed with the patient and his family, and a consensual decision can be made, taking into account his personal situation and his wishes (where is the patient's right to autonomy?). Or even its use could be restricted for this group of patients until more safety data are available. But no, the EMA has gone with the broad brush and has unceremoniously denied it. In a veiled way, it is implied that the economic impact of the introduction of these treatments and the modifications that would have to be made to implement them does not compensate. Unfortunately, I believe that, in the end, this is what has prevailed.
My personal view of these treatments is as follows. They are not a panacea, but there are groups of patients who can benefit from them with a low (and acceptable) rate of side effects. And we cannot deny them that opportunity, it is unethical. We are providing treatments for incurable diseases, such as some cancers, which are much more toxic and dangerous. It is the patient who, faced with his or her clinical situation, with no other options, decides, advised and accompanied by the medical team attending him or her. This is a neurodegenerative disease without treatment, don't our patients deserve the opportunity to decide if it is worth the risk with minimum guarantees? Are Alzheimer's patients second-class patients?
Well, if this is clear to us, let us put in place the measures to get it right: a European registry of all patients treated in specialized centers, with experience in the use of antiamyloids, which can ensure a correct indication and adequate monitoring of side effects. In this way we will obtain the evidence of its long-term effect, since we will only obtain it from real clinical practice. No private laboratory is going to pay for a clinical trial of 5 or more years, which is what would really be needed to see major effects (this has already been modeled for some time). With this decision we will leave this data to be provided by the clinical experience of the other countries where it has already been approved. Or from wealthy Europeans going to the US for treatment, as John Hardy has commented. Our patients will have to wait at least 4-5 years for this and it will already be too late for them.
Conflict os interesnt: “I am participating in a clinical trial with lecanemab promoted by Eisai and I have participated in an advisory board with them”.
Lecanemab EMA - Robert Howard
Robert Howard
Professor of Old Age Psychiatry, UCL Division of Psychiatry, UCL
Based on the clinical trial evidence of only very modest efficacy, that would just not be noticeable in an individual person with Alzheimer’s disease and that cannot be considered clinically meaningful by any objective measure, and the real risks of harms from brain swelling and bleeding, EMA have made the right decision in my opinion.
We all want to see treatments for this terrible condition. I have worked in the field for more than 30 years and am as impatient as anyone for something to offer my patients and their families. But I don’t want them to be given false hope or to be exposed to a treatment that is more likely to harm than to help. EMA have looked carefully at the trial data and their decision reflects their conclusion that lecanemab is more likely to harm people with Alzheimer’s disease than to help them. On behalf of my patients and colleagues, I would want to thank them for their work and for coming to what must have been a difficult decision to reach and to express.