Reaction: two analyses review efficacy of faecal transplants for treating ‘C. difficile’ infections and irritable bowel diseases
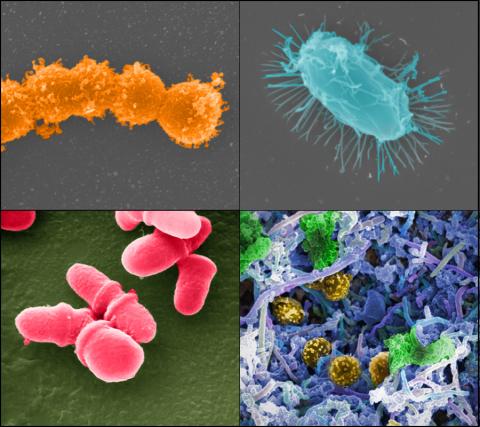
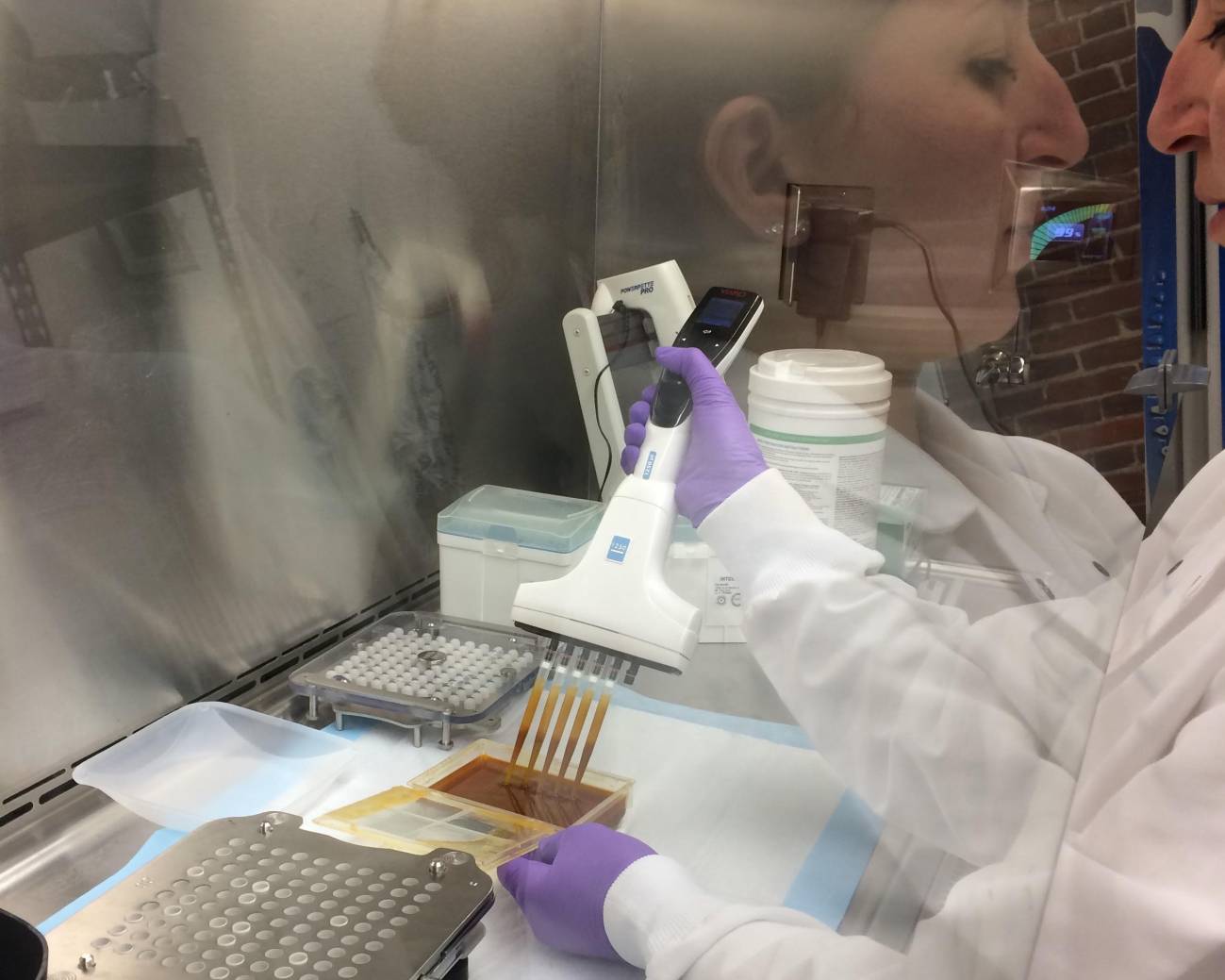
Faecal microbiota transplantation can be administered by oral capsules, colonoscopy or rectal enema, among other routes. Two meta-analyses evaluate its benefits and side effects for treating two types of disease. The first focuses on recurrent infections with Clostridioides difficile, a bacterium that can cause very severe diarrhoea; it includes six studies in Europe and North America involving 320 adults and concludes that in immunocompetent people, faecal transplantation is more effective than antibiotics. The second focuses on irritable bowel diseases, such as ulcerative colitis and Crohn's disease; it includes 12 studies with 550 participants and has less clear results.
Trasplante microbiota - Toni Gabaldón
Toni Gabaldón
ICREA research professor and head of the Comparative Genomics group at the Institute for Research in Biomedicine (IRB Barcelona) and the Barcelona Supercomputing Center (BSC-CNS).
These papers present a meta-analysis of several studies on the efficacy and safety of faecal microbiota transplantation in two indications: Clostridium difficile infection and irritable bowel disease (including ulcerative colitis or Crohn's disease). The methodology is correct for a meta-analysis, which considers data from several different studies. Even adding up all the studies considered, the sample size is moderate (500-600 persons) considering that the study cases are not homogeneous; therefore, more research is needed.
In the first case (C. difficile), it is observed that faecal transplantation leads to a greater remission of symptoms than with alternative treatments (antibiotics), at least in immunocompetent individuals. In the second case, the results are more uncertain and it is suggested that there may be a positive effect in ulcerative colitis, but the evidence is not considered proven. In both cases, the study of possible adverse effects - especially in immunocompromised individuals - would require longer and more extensive follow-up.
This type of treatment is increasingly reaching the clinic and these results are consistent with the findings of other studies. It may work in these types of disorders where there are no effective treatments, but there is a lot of inter-individual variability, both in terms of the donor of the faecal microbiome and the recipient. I believe these approaches will improve when we have a more detailed understanding of the interactions between the microbiome and our immune system. Surely the technique will evolve towards more selective transplants, no longer of an entire faecal microbiota, but of defined microbial communities, different according to the patient and the indication. To get there, we still have a long road of basic and applied research ahead of us.
Minkoff NZ et al.
- Research article
- Review
- People
Imdad A et al.
- Research article
- Review
- People