Aspirin reduces the formation of metastasis in mice, according to a study
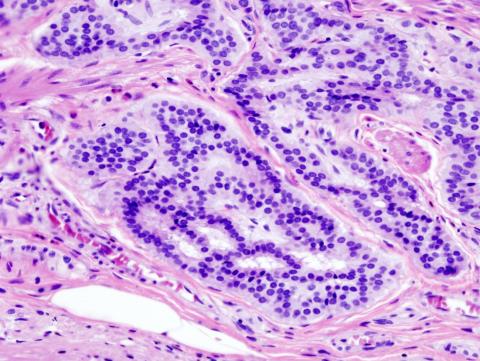
An international team has found that aspirin is capable of reducing the appearance of metastasis in mice, by enabling the activation of T lymphocytes capable of recognising tumour cells. The research showed that several different mouse cancer models — including breast cancer, colon cancer and melanoma — treated with aspirin showed a lower rate of metastasis in other organs, such as the lungs and liver, compared to untreated mice. According to the authors, who publish the results in the journal Nature, ‘the finding paves the way for the use of more effective anti-metastatic immunotherapies’.

Ignacio Melero - aspirina metastasis EN
Ignacio Melero
Professor of Immunology at the University of Navarra, CIMA researcher and co-director of the Department of Immunology and Immunotherapy at the Clínica Universidad de Navarra.
This article adds interesting evidence to a recurring theme in cancer immunotherapy. Several prostaglandins, lipid mediators of inflammation, are immunosuppressive in the context of tumours. This has been demonstrated with prostaglandin E2 produced by the tumour cells themselves in pioneering work by the groups of George Coukos (Lausanne) and Santiago Zelenay (Manchester). Another of these prostaglandins, called thromboxane A2, is produced by activated platelets and, in fact, is involved in platelet aggregation to form thrombi. Prostaglandin synthesis can be blocked by drugs such as aspirin, which inhibit a crucial enzyme in its synthesis.
In this interesting piece of work published in Nature, the authors from the University of Cambridge are able to demonstrate an interesting mechanism according to which platelets, by producing thromboxane A2, are able to interfere with the activation of immune system cells (T lymphocytes) capable of recognising and destroying tumours. This phenomenon is especially relevant for tumour cells that enter the bloodstream with the risk of generating metastasis. In this context, tumour cells are particularly susceptible to elimination by cells of the immune system and appear to use thromboxane A2-producing platelets as bodyguards.
The deductive research is brilliant. They had previously discovered a factor that facilitates metastasis in mice and in the screening a regulatory protein appeared that is relatively unknown but whose levels increase with thromboxane A2. From there, they found that thromboxane favours metastasis through an immunosuppressive mechanism and through this experimental route they observed that aspirin and other prostaglandin synthesis inhibitors decrease the efficiency of metastasis.
What is missing from the article is the demonstration of the same phenomenology between human platelets and lymphocytes. The data suggest that we should explore whether low-dose aspirin (antiplatelet dose) consumption decreases the likelihood of metastasis in cancer patients or whether patients receiving aspirin are less frequently diagnosed at the metastatic stage.
Previous studies, to which this one is now added, give reasons for carrying out clinical trials in which the synthesis of prostaglandins is blocked in the context of the immunotherapy treatments that we routinely apply to patients.
Ramón Salazar - aspirina metástasis EN
Ramón Salazar
Head of Medical Oncology at the Catalan Institute of Oncology (ICO), head of the Colorectal Cancer Research Group, Oncobell programme (IDIBELL) and associate professor of Medicine at the University of Barcelona
The study fulfils all the methodological and technological criteria for experimentation in preclinical models.
It explains a new mechanism of action of aspirin on the inhibition of T-lymphocyte activation, but does not influence current clinical recommendations.
The greatest limitation is the same as always in preclinical research and that is that what happens in preclinical models does not necessarily happen later in the human organism. In fact, in several randomised adjuvant trials in colon and breast cancer, aspirin has not improved relapse-free survival or overall survival.
Lanas - aspirina
Ángel Lanas
Professor at the Faculty of Medicine of the University of Zaragoza, head of the Digestive Service of the Hospital Clínico Universitario Lozano Blesa of Zaragoza and scientific director of the Instituto de Investigación Sanitaria de Aragón (IIS Aragón)
I think the study is excellent, as it explores a pathogenic pathway related to metastasis and the effect of aspirin (aspirin, ASA) that, to my knowledge, had not been explored in such depth and in such a complete manner at the experimental level. The study is of high quality; otherwise it would not have been published in Nature.
We have been investigating the effect of ASA on digestive cancer and, in particular, colon cancer for many years. We have made interesting interesting contributions with some of the authors of this paper. We have known from the epidemiological point of view, for many years, that people who take ASA daily have a lower risk of cancer and a lower mortality associated with cancer. Relevantly, we knew that taking ASA, even after the diagnosis of cancer, was associated with a lower risk of metastasis. The suspicion that this effect was platelet-dependent and possibly related to immunity has always been present, but the mechanism was not clear beyond plausible hypotheses. This work represents an important step towards confirming this hypothesis and opens up new therapeutic avenues associated with immunotherapy, which is providing such good results in many tumors.
As always, it should be noted that complexity in humans is greater and less controllable than in experimental conditions. We are clearly moving towards personalized medicine in which cancer treatment will be individualized. It is quite possible that this very interesting effect will be seen only in some types of cancer that express a specific molecular profile that will have to be better defined.
Conflicts of interest: “I have been advisor to Bayer AG”.
Yang et al.
- Research article
- Peer reviewed
- Animals