Reactions: Clinical trial tests gene therapy in severely immunodeficient children
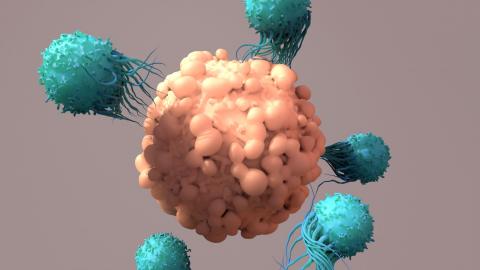
Bubble boy syndrome is a very serious condition caused by combined immunodeficiency. It is sometimes caused by certain mutations in the gene that codes for the Artemis protein. A phase I-II clinical trial has tested a gene therapy that adds a correct copy of the gene. The results are published in the journal NEJM.
Luis Ignacio González Granado - niño burbuja
Luis Ignacio González Granado
Specialist in immunodeficiencies and Associate Professor of Paediatrics at the Complutense University of Madrid
The paper published by Cowan et al. is the first work in humans to demonstrate the possibility of correction of this disease by gene editing. In this single-centre phase I/II trial, the authors demonstrate the safety and efficacy of this treatment for a specific type of severe combined immunodeficiency (SCID, commonly known as bubble boy disease) due to Artemis deficiency, using a lentiviral vector.
The study describes the outcomes of ten patients lacking an HLA-identical sibling for haematopoietic stem cell transplantation (HSCT) between June 2018 and September 2021, with monthly follow-up for the first six months and quarterly until 24 months. The methodological quality is optimal and in line with clinical trials of gene therapy in this group of diseases. The study design consists of two phases. In the first phase, treatment success is measured by the safe administration of the modified cells and the safe use of busulfan 42 days after infusion. Safety is measured by the absence of serious adverse events and reconstitution conditions derived from the introduction of the vector into the cells in this type of assay, as well as transduction efficiency. The second measure of treatment success, already in the second stage, measures the reconstitution of functional T cells twelve months after the procedure.
SCID is a paediatric emergency and affects approximately one in 35,000-50,000 newborns. In the United States, since December 2018, every newborn is screened quickly and reliably in conjunction with endocrine-metabolic testing at 48 hours of age, allowing early identification of SCID.
It is a fatal disease without treatment in the first 2 years of life due to the development of infections, autoimmunity or cancer.
Artemis deficiency (protein encoded by the DCLRE1C gene) is a type of SCID due to a defect in the DNA repair system of non-homologous end-joining (NHEJ) that occurs, among other causes, due to the effect of ionising radiation. These patients are therefore at risk not only of immunodeficiency but also of cancer, as we know from patient cohorts and in vitro radiosensitivity and repair studies.
The preparation of the patient for the treatment referred to in the NEJM article requires the administration of a small dose of chemotherapy to ensure the best possible haematopoietic progenitor attachment compared to earlier studies in this field (both gene therapy and HSCT, where the absence of conditioning implied very poor immune reconstitution - i.e. insufficient replacement due to the presence of previous progenitors with the disease). In HSCT, the doses required are 4 times higher than in gene therapy. Considering the risk of malignancy in these patients, the use of lower doses of chemotherapy is justified to promote effective progenitor attachment with the least possible toxicity, as demonstrated by the authors in this paper.
From the point of view of efficacy, assessed in terms of immune reconstitution, the study demonstrates recovery of T, B and NK lymphocytes. In four out of six cases, patients become independent of gamma globulin administration (at 24 months follow-up), which is necessary in the pre-treatment period to avoid serious infections. This result is equal or superior to that obtained with HSCT.
In addition, immunological recovery makes it possible to suspend prophylactic treatments prior to the procedure to avoid serious, even life-threatening, infections. Such infections by viruses, bacteria, fungi and/or parasites even condition the outcome of treatment, as can be seen in the ART010 patient, with poor reconstitution possibly due to previous cytomegalovirus infection with antiviral resistance (Table 1).
The high rate of autoimmune haemolytic anaemia (four out of nine at one year follow-up) necessitates long-term follow-up of this complication, probably related more to the underlying disease (it is a possible complication of SCID, as is the case in the severe combined immunodeficiency subtype, X-linked), as the authors acknowledge in the limitations at the end of the article) than to the gene therapy procedure.
The poor cell attachment in the myeloid lineage (the insertion of the vector with the corrected gene into cells other than lymphocytes) (Figure 3) is a phenomenon resulting from the reduced use of busulfan, which may need to be improved in the future. More follow-up time is needed to know what implications this may have.
In summary, the work represents a step forward in the development of safer and more effective treatments for bubble children with this particular type of disease.
Taking into account the World Health Organisation's criteria for neonatal screening (Wilson and Jungner, 1968), one of the requirements for the implementation of a screening programme is the existence of a curative treatment with the least possible toxicity. The results of the present study support the possibility of offering patients with this disease a curative treatment with the lowest possible toxicity.
What does this mean for children in our country who may have this disease? Although the strategy of screening at birth - together with the rest of the endocrinometabolic tests - has been shown to be cost-effective, in Spain it has only been implemented at the population level in Catalonia since 2017. Several Autonomous Communities have expressed interest or have recently implemented it in their legislation as a step prior to de facto implementation.
Pere Soler - niño burbuja
Pere Soler Palacín
Head of the Paediatric Infectious Pathology and Immunodeficiency Unit of the Vall d'Hebron Children's Hospital in Barcelona.
This is excellent work carried out by a team at the forefront of the field. The data provided are robust and, although ten patients may seem very few, in entities as rare as this type of severe combined immunodeficiency (SCID) they are more than correct.
This work adds another SCID to the group of primary immunodeficiencies that can be treated by gene therapy. This technique, when it works properly as in this case, usually provides similar or even better results than haematopoietic precursor transplantation with less toxicity, as it does not infuse "external" cells into the patient but genetically modifies the patient's own cells.
An important theme of the study is that almost all of the patients included had been diagnosed by neonatal screening, so gene therapy was applied in patients free of complications of their disease. This point further reinforces the importance of the neonatal screening-gene therapy pairing in the treatment of these and other genetic diseases.
The main limitation of the study is the relatively small number of patients who will benefit from this treatment, because for the remaining SCIDs with different genetic defects, studies with the same characteristics will have to be performed. Similarly, as the authors comment, longer follow-up is needed to determine the benefit of treatment for non-immunological defects in SCID.
Óscar de la Calle - inmuno niño burbuja EN
Óscar de la Calle-Martín
Specialist in Immunology at the Hospital de Sant Pau in Barcelona and secretary of the Spanish Society of Immunology
The study is excellent and the results are spectacular: they have achieved immune reconstitution in all cases (10/10). The article is scientifically very sound. The follow-up is very well done and the medical and immunological results are consistent. The procedure achieves results superior to those achieved with the standard treatment, bone marrow transplantation.
Primary immunodeficiencies were the first genetic diseases to be treated by gene therapy, especially the most severe forms, which are lethal without treatment, called Severe Combined Immunodeficiencies (SCID). Currently, the lentiviral vectors used, such as the one used in this case, ensure a very high safety margin, with fewer side effects than the classic treatment, haematopoietic progenitor transplantation. This has made them the first-line treatment in countries with this technology (USA, UK, France, Germany, Italy, etc.).
This is not a very novel therapy, as it has been previously tested in other primary immunodeficiencies (SCID-X, WAS, etc.) with similar results. The novelty is the pathology in which it has been used, but its use in this particular case is limited to this single disease, which is very rare.
As for the limitations, there are basically two. Spain is the only large country in the European Union that does not have gene therapy for this type of pathology (primary immunodeficiencies) or similar (thalassaemia or other genetic blood diseases). This is due to the fragmentation of our health system, as well as the lack of a National Immunology Centre, which is available in other neighbouring countries, even those with a lower GDP than ours.
The other limitation is due to the fact that it is a very rare variant of SCID (SCID-ART, for the Artemis protein), although in the USA it is somewhat more frequent as it is found in people of Navajo/Apache origin. There are very few cases in Spain. Each variant of the disease can only be treated with a gene therapy vector made specifically for each responsible gene. In the case of SCID, more than 40 genes are involved.
Another limitation, although in this case a previous one, derives from the fact that in Spain, with the exception of Catalonia, screening for these diseases is not carried out in the perinatal screening, the famous heel prick test that is performed on all newborns. These treatments have an even more beneficial effect if they are done before the child starts to have serious infections, but they are also effective in children as young as possible. Both are achieved by introducing these studies into the heel prick, as is already done in the USA and in many European countries, as well as in Catalonia.
Alsina - Inmunodeficiencias (EN)
Laia Alsina
Head of the Allergy and Clinical Immunology Department at the Hospital Sant Joan de Déu in Barcelona.
The article is excellent in methodology and format. The NEJM journal is an assurance of its quality and the research team (Dr. Puck) has been a reference in the field for more than 30 years.
Gene therapy is a current therapeutic strategy, relevant and necessary when other therapeutic solutions fail in highly lethal diseases such as SCID [Severe Combined Immunodeficiencies]. They should be able to reach the market like gene therapy for ADA-SCID, another common form of SCID.
The relevance of gene therapy is made clear in this review by the world's leading gene therapist, Professor Alain Fisher: https://pubmed.ncbi.nlm.nih.gov/36434109/
The most important limitations are economic. Also the risk of oncogenesis [tumour development] of any gene therapy, which has not been seen in this trial.
Cowan et al.
- Research article
- Peer reviewed
- Experimental study
- Clinical trial
- People