EMA revises earlier decision and decides to approve lecanemab for Alzheimer's disease
Less than four months after the European Medicines Agency recommended in July not to grant marketing authorisation for Leqembi™ (lecanemab) for the treatment of Alzheimer's disease, the EMA's Committee for Medicinal Products for Human Use (CHMP) has reassessed the available evidence to conclude that the benefits outweigh the risks.

Juan Fortea - lecanemab EMA 2 EN
Juan Fortea
Director of the Memory Unit of the Neurology Service of the Hospital de la Santa Creu i Sant Pau and director of the Alzheimer's Unit at the Fundació Catalana Sindrome de Down
I am extremely pleased with the recent approval of lecanemab by the EMA after reconsidering its decision in the appeal process. This breakthrough represents a milestone for Alzheimer's patients and marks a paradigm shift in their treatment.
Although use will be restricted to a minority in the early stages, it will drive the development of essential diagnostic and therapeutic capabilities, as was the case with stroke units, benefiting all patients, both those who receive the drug and those who do not.
This is excellent news, correcting a worrying decision and bringing Europe back to the forefront of Alzheimer's research and care.
Mercè Boada - lecanemab EMA 2 EN
Mercè Boada Rovira
Neurologist and medical director of Ace Alzheimer Center Barcelona.
This is the news we were waiting for with a certain amount of caution, because the EMA is a very conservative body that evaluates the risk situation of patients very carefully, which was one of the key points here for accepting treatment with Leqembi.
This is the best news we have had this year. Europe needed this news. Europe needed to know that we had the possibility of treating patients, we needed to know that all research in this field would continue and that we understood, as was already done in the document and the paper sent by the European Alzheimer's Disease Consortium, that what had to be very well defined were the restrictions, taking into account the validity and experience of the prescribing centres that have had - even if they had previous experience in clinical trials of monoclonal antibody treatment. This acceptance by the EMA balances the situation so that our patients in Europe and Spain have the same opportunities as others.
Hilary - lecanemab EMA 2 EN
Hilary Evans-Newton
Directora ejecutiva de Alzheimer's Research UK
Today’s decision by the EMA’s advisory committee to reverse its previous stance and approve lecanemab marks an important milestone in the global fight against Alzheimer’s disease. While not a cure, lecanemab is a significant step forward. Lecanemab is among the first treatments proven to slow memory and thinking decline linked to Alzheimer’s, rather than just alleviating symptoms. This progress, however modest, marks a breakthrough in the way Alzheimer’s can be treated.
This decision is aligned with regulators in other G7 countries. The EMA in keeping with the UK, have decided to exclude certain people from receiving lecanemab, including those who carry two copies of a gene called APOE4, as this puts them at higher risk of side effects. Around 15% of people with Alzheimer’s disease carry two copies of this gene. While the drug is not available through the NHS, people across the US and Japan are already receiving lecanemab, with monitoring systems in place to track progress which is improving our understanding of how these drugs work outside of clinical trials. This information will play a key role in guiding future clinical decisions, such as which patients benefit most from the treatments, how long it should be given for, and at what stages of the disease.
While these new Alzheimer's treatments are far from a perfect solution, they open the door to future treatments that will be safer and more effective, bringing us closer to a day when we can slow, stop, and even reverse all forms of dementia. Thanks to decades of research, we’ve made tremendous strides in understanding Alzheimer’s, and research remains our best hope of finally making this devastating disease a thing of the past.
Rob - lecanemab EMA 2 EN
Robert Howard
Professor of Old Age Psychiatry, UCL Division of Psychiatry, UCL
This is in line with what the UK’s MHRA decision, that, in a subset of patients with early Alzheimer’s disease, the benefits of treatment exceed the risks. This is not to say that lecanemab is clinically or cost-effective.
I anticipate that the bodies that determine cost-effectiveness of new drugs within individual jurisdictions will struggle to approve lecanemab for use in their public health systems. The treatment is expensive and benefits are marginal.
John Hardy - lecanemab EMA 2 EN
John Hardy
Professor of Neuroscience and Group Leader at the UK Dementia Research Institute, UCL.
I think this is great news and the right outcome: a restricted approval makes the most sense. In my view, this is the right outcome.
Conflict of interest: "I have consulted for Eisai and for Lilly".
Tara - lecanemab EMA 2 EN
Tara Spires-Jones
Director of the Centre for Discovery Brain Sciences at the University of Edinburgh, Group Leader in the UK Dementia Research Institute, and Past President of the British Neuroscience Association
The news from the European Medicines Agency (EMA) that lecanemab is recommended for treating some people with early Alzheimer’s disease will bring hope to people across Europe affected by Alzheimer’s. However, it is important to note that this treatment is not available to everyone and it is not a cure, people taking lecanemab still have progression of symptoms, albeit more slowly than people without treatment. Further, the treatment comes with risk of brain swelling or bleeding meaning that in addition to frequent drug infusions, people taking lecanemab need brain scans to monitor for side effects.
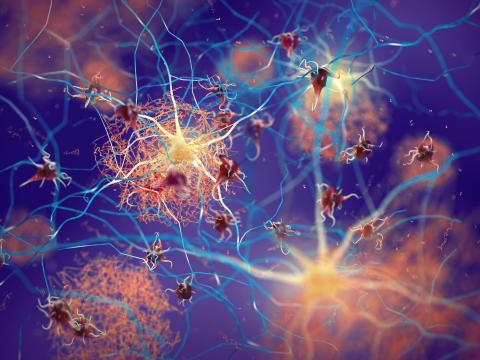
Lecanemab is an antibody that removes sticky amyloid pathology from the brain. In July 2024, the EMA decided that the benefits did not outweigh the risks of treatment; however a new re-examination of the data by their Committee for Medicinal Products for Human Use reversed this opinion and recommends granting marketing authorization for some people. The recommendation is only for people with who do not carry two copies of the risk gene called apolipoprotein E epsilon 4 (APOE4). People with 2 copies of the APOE4 gene are at higher risk of potentially dangerous side effects. Around 1 in 50 people have 2 copies of the APOE4 gene in the general population. The new conclusion from the EMA is that the benefits of lecanemab treatment outweigh the risks for people with zero or one copies of the APOE4 gene.
Declarations of interest: "I have no conflicts with this announcement but have received payments for consulting, scientific talks, or collaborative research over the past 10 years from AbbVie, Sanofi, Merck, Scottish Brain Sciences, Jay Therapeutics, Cognition Therapeutics, Ono, and Eisai. I am also Charity trustee for the British Neuroscience Association and the Guarantors of Brain and serve as scientific advisor to several charities and non-profit institutions".
Pablo - lecanemab EMA 2 EN
Pablo Martínez-Lage Álvarez
Neurologist, scientific director of the CITA-Alzheimer's Foundation
I think it is to be welcomed that the EMA has rectified a previous decision that had been taken on flimsy grounds. It took the decision on the basis that the beneficial effect of this drug did not outweigh the risks of possible side effects. It was an argument that was not supported by the data from the clinical trials that have been done.
It is a drug that manages to change the natural history of the disease in its earliest stages, when there is no dependence or dementia yet. It changes the progression of the disease in people who are diagnosed with Alzheimer's when they are still living a normal or near-normal life. Therefore, it contributes to the promotion of people's autonomy, which is what the Dependency Law is all about, which is not about dependency, but about the promotion of autonomy.
It is true that this treatment will not be indicated for all people with Alzheimer's, but only for people diagnosed very early, with a diagnosis based on the use of biomarkers, either by puncture or PET. The news has to be given with this caution, it is not a treatment for everyone.
There is something important: we Europeans working on Alzheimer's felt a little embarrassed when talking to researchers in other countries where it had been approved, such as the US and Japan, because our European Medicines Agency had taken an attitude that could be interpreted as ‘well, let the drug be tested in other countries and if people don't die there and we see the effect, then we will apply it here’. This is to be congratulated, Europe is jumping on the bandwagon of research and its own guidelines. Let us remember that, in 2011, the European Commission and the European Parliament came out in favour of declaring Alzheimer's a priority disease, with an opinion that spoke of research into new drugs, the creation of diagnostic units, etc.
I understand that the Spanish Agency for Medicines and Health Products (AEMPS) will follow the guidelines of the European Medicines Agency (EMA), which, as I say, are based on clinical trial data. Our 17 health systems will have to prepare to facilitate early diagnosis for people, they will have to prepare to decide whether to fund it or not. Now public-private creativity comes into play so that the company and the administrations agree on prices that are reasonable according to the calculations that are already more than done and published. I trust in the creativity of our politicians so that they know how to agree on affordable prices and that not only is marketing approved in Spain, but also that the drug reaches people's homes, that it is not a treatment for the rich.
Jordi Pérez Tur- lecanemab EMA 2 EN
Jordi Pérez-Tur
Research scientist at the Public Research Organisation (PRO) at the Institute of Biomedicine of Valencia of the Spanish National Research Council (CSIC)
After 20 years without major advances in the treatment of Alzheimer's disease (AD), some hope seems to be emerging. The use of monoclonal antibodies against the amyloid peptide is a first, small step towards effective treatments for the disease.
First, the caveats. This treatment has been shown to have some efficacy provided it is administered to individuals in the early stages of the disease or with a diagnosis of mild cognitive impairment, a clinical form that in many cases is a stage prior to Alzheimer's disease itself, and who, moreover, do not carry any copies of the E4 allele in the APOE gene or, at most, are heterozygous for this allele, i.e. carry a single copy. In other words, it is a treatment that offers its maximum benefit in very early cases of the disease and in a subgroup of those with the disease. Given the high frequency of carriers of 2 copies of the E4 allele in this condition, it is clear that this is not a disruptive treatment. However, it is a much needed, long awaited and welcome development.
It is now 25 years since experimental models of AD began to be treated with antibodies directed against the amyloid peptide, the main component of a type of lesions seen in the brains of patients. In these models, the results were spectacular. The lesions disappeared over time and the treated animals performed better on memory tests. However, these results did not immediately translate to humans. It has taken intensive laboratory work to obtain formulations that are sufficiently effective to gain approval from regulatory agencies in several countries around the world, including Europe, albeit with the conditions outlined above.
However, a few months ago (July 2024), the European Medicines Agency refused to approve the use of this same antibody for the treatment of AD. Why is its use allowed now? Simply because at the time it was intended for use in all patients in the early stages of the disease and it was seen that this treatment harmed rather than benefited the patients as a whole, as a significant increase in the occurrence of oedema or cerebral haemorrhages was observed in the group using the antibody. That is, the benefit observed in terms of AD progression was less than the risk of severe symptoms associated with the treatment, not the disease.
In a subsequent analysis, the pharmaceutical companies behind the treatment (Eisai and Biogen), saw that the treatment was more effective in a subgroup of patients (those with one or no copies of the E4 allele in the APOE gene). This new way of looking at the data has now allowed the treatment to be approved subject to the conditions outlined above: patients in the early stages or with a diagnosis of mild cognitive impairment and carrying a maximum of one copy of the E4 allele. That said, the effectiveness of the treatment, contrary to what might be thought, does not lie in stopping or reversing the disease. The effect achieved is to slow the progression of the disease for at least the 18 months that the clinical trials studied for the approval of the use of lequembi as a treatment for AD have lasted.
This treatment, on the other hand, requires intensive follow-up and has an administration that implies the need for the patient to be close to a centre that can carry out this follow-up before, during and after treatment. This also opens up a discussion about how to ensure access for all those patients who could benefit from it. Not everywhere, patients can have access to tests as simple as APOE genotyping to see if they are candidates for treatment. From this point, I repeat, the simplest to consider from a technical point of view, we can clearly see how it is necessary to establish mechanisms that allow the treatment to reach all those patients who can benefit from it without the postcode being a limiting factor in this decision.
In summary, we are at a hopeful moment in that there is already a treatment that allows a certain slowing down of the progression of a disease as complex as AD, and which reinforces the opinion that many researchers have defended for a long time: that the amyloid peptide is a good candidate for the development of therapies. Although the results are unspectacular, given that the process is not reversed but slowed down, it is an important step in that direction. Let us hope that progress continues to be made in this direction without this implying the abandonment of other research based on alternative hypotheses to that of the amyloid cascade, which may also contribute to improving the therapeutic arsenal available to us in the hopefully nearer rather than more distant future. The complexity of the disease, reflecting pathological processes that begin decades before the first symptoms manifest themselves, will most likely only be resolved with equally complex treatments involving several of the molecules that are related to the disease.
Marc Suárez - lecanemab EMA 2 EN
Marc Suárez-Calvet
Researcher at the Barcelonabeta Brain Research Center and the Neurology Service of the Hospital del Mar (Barcelona)
The recommendation by the EMA's Committee for Medicinal Products for Human Use (CHMP) to approve lecanemab in Europe represents a promising advance in the fight against Alzheimer's disease. This treatment, the first to show the ability to slow disease progression, is indicated for patients in early stages and with a specific genetic profile, excluding those with two copies of the APOE4 gene due to a higher risk of side effects. Furthermore, its administration will be controlled through a limited access programme to ensure safe and appropriate use.
Importantly, this recommendation does not imply immediate availability of the drug across Europe, as each country will have to decide whether to include it in its public health system. While lecanemab offers modest efficacy and is expected to initially benefit a small number of patients, its approval opens the door to more effective and safer treatments in the future, as well as boosting research and development of new therapies and advancing the diagnosis of Alzheimer's disease.