CRISPR used for the first time to treat a rare metabolic disease in a baby
A team from the Children's Hospital of Philadelphia and Penn Medicine (United States) has successfully treated a baby diagnosed with a rare genetic disorder using personalised CRISPR gene editing therapy. The baby, known only by the initials KJ, was born with a rare metabolic disease known as severe carbamoyl phosphate synthetase 1 (CPS1) deficiency. After spending the first months of his life in hospital on a very restrictive diet, KJ received the first dose of his tailored therapy in February 2025, between six and seven months of age. The treatment, which is being used for the first time for this type of disorder, was administered safely, and the baby is now growing well and improving. The case is detailed in a study published by The New England Journal of Medicine (NEJM).

Marc Güell - CRISPR EN
Marc Güell
Coordinator of the Translational Synthetic Biology research group and full professor at Pompeu Fabra University (UPF)
Does the press release accurately reflect the study?
‘Yes.
Is the study of good quality?
‘It seems to me to be a study of the highest quality and totally extraordinary. In fact, I was deeply moved to read it. It reflects the great potential of gene editing for therapeutic purposes. The researchers and clinical team have done a very thoughtful design with all the precautionary steps that the situation allows: characterisation of mutations, design of editors to correct, measurement of efficiency and off-target [unwanted effects], as well as testing the reagents in cell and animal models. Extraordinary work in record time.
How does this work fit with the existing evidence?
‘Great proof of concept that it is not impossible to treat very rare diseases at the individual level.
Are there any major limitations to be taken into account?
‘We will have to characterise the precision gene editing process in the future (patient safety permitting). For now, it has been possible to measure the positive clinical effects, but for patient safety reasons it has not been possible to obtain liver tissue to characterise the efficiency of gene editing.
It's a great demonstration, but it's also worth noting that this correction has been done in the liver; other tissues are much more difficult to gene edit, for now.
What are the implications for the real world?
‘Individualised, tailor-made therapies for a single patient are no longer a dream. Obviously, the process followed is of very high complexity and will require a lot of work to see how to scale it up and expand it to other cases. In any case, this work sheds a lot of light on the future’.
Lluís Montoliu - CRISPR EN
Lluís Montoliu
Research professor at the National Biotechnology Centre (CNB-CSIC) and at the CIBERER-ISCIII
Base editors represent the second generation of CRISPR tools and have been developed by David Liu, a researcher at the BROAD institute, who has also developed the third generation of editing tools, the quality editors. The base editors were created in 2016 by David Liu by combining two activities that had never been together in any living being throughout evolution, which underlines the talent and vision of this researcher in creating from scratch tools capable of chemically changing the identity of nucleotides, without requiring cutting the DNA double strand, which is the characteristic limitation of the first-generation CRISPR tools (and which therefore generates so much diversity of results, not all of which are necessarily correct). There are at least two types of base editors, depending on whether they can convert an A to a G (called ABE) or a C to a T (called CBE) in a precise sequence of the selected gene.
Base editors were used to cure the T-cell acute lymphoblastic leukaemia of Alyssa, a medically hopeless 12-year-old British girl who was resistant to chemotherapy and radiotherapy treatments, but nevertheless managed to pull through with the use of these base editors, which, in this case, were used to inactivate several genes, interrupting their translation, before proceeding to give her CAR-T cell therapy.
Base editors have also been used to inactivate the PCSK9 gene , which encodes the repressor of the low-density lipoprotein (LDL) receptor, which transports cholesterol in the blood, and whose therapeutic effect is to significantly lower serum cholesterol as a potential therapy for people with familial hypercholesterolaemia. This study was validated preclinically in mice, in non-human primates and is currently being evaluated in a clinical trial. In both the case of Alyssa and the PCSK9 gene, base editors were used to inactivate a gene by changing a codon in the sequence coding for an amino acid to a stop codon, which interrupted the synthesis of the protein, which, being truncated, was unable to perform its function.
The work with the base editors to inactivate the PCSK9 gene was led by researcher Kiran Musunuru, from the University of Pennsylvania and the Children's Hospital of Philadelphia (USA). His team now reports in the New England Journal of Medicine (NEJM) the use of base editing technology not to inactivate, but to correct a mutation in a gene associated with a severe congenital rare disease, a metabolic disorder called deficiency in the enzyme carbamyl phostate synthetase I (encoded by the CPS1 gene), which is an essential urea cycle protein responsible for removing residual ammonium from protein metabolism. Mutations in the CPS1 gene inactivate this enzyme and cause severe symptoms in children within days of birth, with vomiting, hypothermia, hypotonia, epileptic seizures and coma, and may lead to death. Treatment involves dialysis to eliminate ammonium, reduction of dietary protein and eventually liver transplantation, which, however, does not resolve the neurological disorders that also occur. It affects about 1 in 300,000 births, about half of whom will eventually die.
In this case, researchers diagnosed the presence of two mutations (one of paternal origin and one of maternal origin) in a child affected by CPS1 deficiency. One of them was chosen to be treated with an ABE-based editor. The strategy was validated first in cultured liver cells and then in a mouse model. All this occurred during the first six months of the child's life. The researchers applied to the regulatory agency (FDA) for approval of this therapy for a single patient and, after obtaining approval, proceeded to administer the base publishers encapsulated in lipid nanoparticles (the same ones used for the covid-19 mRNA vaccines) on two occasions, at months 7 and 8 of life. The child, despite suffering several viral infections, recovered and reduced his blood ammonium levels while increasing the presence of protein in his diet without causing harmful effects. The researchers have been able to assess little else about the treated child, as liver biopsy is not recommended at this age. Nor about the safety of the treatment, about the possible other modified genome sites or about the unlikely (due to previous experiments on mice and macaques) editing of the child's gonads (testicles), which would mean that he could pass on his edited DNA to his offspring. Medium- and long-term study of the treated patient, as well as other similar patients, will be necessary to draw more robust conclusions.
This is a paradigmatic case of developing an ad hoc therapy for a mutation in a single person, a single patient. An economically and ethically debatable initiative (because of the massive and always limited resources that must be invested to treat a single person) and hardly scalable or universalisable, given that each patient will carry different mutations. From the experimental point of view, the approach of single-patient therapies is very risky, given that the lack of controls or variables means that only the success of the treatment can be explained, when it occurs, but not its failure, which may be caused by multiple factors that have not been controlled for in the experimental design. The FDA allows such experimental treatments in cases of very serious diseases, such as CPS1 deficiency, which are incurable and life-threatening.
The researchers anticipate a near future in which these treatments will become more common and even routine. They also predict that, due to previous experience, validation in mice and macaques will no longer be necessary and the patient will be treated after validation of the strategy in cell models only. I consider these to be very optimistic and ambitious wishes, which may have to be revised if success does not follow these pioneering treatments. The important question that the article does not address is the accessibility and affordability of these treatments for children with these diseases. How much will this treatment cost? Where can it be administered? How many children will these new individual therapies reach?
Fernando Civeira Murillo - CRISPR EN
Fernando Civeira Murillo
Professor of Medicine and Head of the Lipid Research Group at the University of Zaragoza
Does the press release accurately reflect the study?
‘I think the press release is very good and accurately reflects the problem and the solution provided by the paper’.
Is the study of good quality?
‘The study is excellent and only has the limitation that the follow-up is short, only a few months, and we will have to wait to see how the child evolves.
How does this work fit in with the existing evidence?
‘Perfectly, it is the future. Gene editing à la carte, individualised for each pathogenic variant responsible for the disease.
Are there any major limitations to be taken into account?
‘The participating centres are world leaders in the technology. The limitation is time, as a severe disease that does not allow for delays in doing further animal testing and experimentation with the therapy’.
What are the implications for the real world?
‘Huge. Probably in a few years the vast majority of severe monogenic diseases will disappear thanks to gene editing’.
Gemma Marfany - CRISPR EN
Gemma Marfany
Professor of Genetics at the Universitat de Barcelona (UB) and head of group at CIBERER
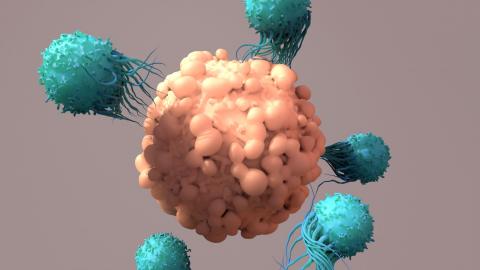
This is the first case of a fully customised therapy, for a single baby (what is called ‘n of 1 therapy’), treated in vivo with a base-editing therapy for a very severe ultrarare disease. The disease causes the accumulation of ammonium, which is highly toxic to neurons and can lead to death in the first months of life. With the help of several leading biotech companies, a novel and very precise strategy has been designed to uniquely modify the mutated nucleotide in the gene to reverse the effect, and instead of a truncated protein, produce the complete protein. In addition, instead of using therapeutic viruses, lipid particles have been used to deliver the gene-editing system to the liver, in three doses within weeks of each other, avoiding an unwanted immune response and achieving remission of the most dangerous symptoms, reducing palliative medication and allowing incorporation of a normal diet.
It is truly a unique case, a successful proof of concept, designed and applied in record time, in which researchers and clinicians have not skipped a single preclinical step, as they have generated human cellular models and also a humanised mouse model with the patient's mutation to test the safety of the dose and the efficiency of the therapeutic strategy. In addition, they have had all the approvals from the relevant bioethics committees. It seems to me to be a scientific ‘miracle’ that has made it possible to cure a very rare severe disease, and provides knowledge to treat many other diseases.
Miguel Ángel Moreno-Mateos - enfermedad metabólica bebé CRISPR
Miguel Ángel Moreno-Mateos
Tenured scientist CSIC & PI, Andalusian Center for Developmental Biology, CSIC-Pablo de Olavide University
Since the emergence of CRISPR-Cas technology, progress has been made to develop a variety of tools that have the potential to contribute to the cure of many genetic diseases. This work demonstrates how, by detecting a specific congenital disease in the first days after birth, a robust protocol can be implemented with the ultimate goal of curing, at least partially, a patient with a particular genetic alteration that causes a rare disease. This protocol contains several steps, including i) characterization of the mutation or mutations that cause the disease, ii) design and comparison of the efficiency of various CRISPR-Cas approaches, which in this case are based on base editing and include various Cas proteins with different DNA recognition capabilities, iii) genetic and physiological safety testing of CRISPR-Cas reagents and lipid nanoparticle-based complexes both in vivo and in vitro, and iv) finally, targeted treatment in the patient's liver in two doses seven months after birth, following approval by the relevant agencies.
Although this has been a very specific approach, partly motivated by the devastating nature of the disease, it represents a milestone that demonstrates that these therapies are now a reality. In any case, as the article reports, the patient will be monitored for a long time to ensure his well-being and determine whether additional doses are needed to further improve the symptoms of the disease.
On the other hand, given the risk involved and as the article itself acknowledges, the percentage of gene editing in the patient himself and any possible unwanted edits have not been evaluated, although they were determined in in vivo and in vitro studies. However, based on the physiological results, everything indicates that, at least so far, the therapy has been successful and has significantly improved the patient's quality of life.
In summary, this work is proof of principle for a rapid and effective protocol for CRISPR-Cas therapies for the cure of human diseases in general and so-called rare diseases in particular, opening the door to other similar treatments in the near future.
Conflict of interest: “I have collaborated with one of the authors of the paper, Benjamin P. Kleinstiver, with whom I published a research paper three years ago.”
Musunuru et al.
- Research article
- Peer reviewed
- Case study